Could a widely used metabolic therapy carry hidden long term risks for patients?This article examines why clinicians and patients ask this question as incretin based therapies gain rapid use for diabetes and weight loss in the United States.
We synthesize mechanistic signals animal findings, real-world claims analyses, and randomized trial results to show where evidence is clear and where uncertainty remains.
Rodent thyroid findings prompted safety labeling yet human biology differs in receptor response and calcitonin release. Claims based studies generally show odds ratios near one for pancreatitis, but wide confidence intervals and short follow-up limit firm conclusions.
Pancreatic cancer develops over decades so short term data may miss rare or delayed effects. This article maps epidemiology mechanisms trials practical prescribing guidance, and research priorities to help clinicians weigh metabolic benefits against potential risks.
Key Takeaways
- Scope: We review mechanistic, preclinical, and clinical evidence to clarify safety signals.
- Species gap: Rodent thyroid results do not directly predict human risk but justify caution.
- Data limits: Claims analyses show no clear pancreatitis increase, yet confidence intervals are wide.
- Latency: Pancreatic carcinogenesis is slow; long follow-up is essential for assessment.
- Practical view: Balance metabolic and quality-of-life benefits with rare safety concerns when advising patients.
Executive Summary What the Latest Data Say About Risk Benefit and Signals
This concise summary highlights what clinicians and patients in the United States need to know about risk, benefit, and remaining uncertainty.
Bottom line: Contemporary studies show clear metabolic and weight benefits for treatment of obesity and diabetes while confirmed malignancy risks remain unproven. Large claims analyses report pancreatitis odds ratios near one versus other glucose lowering therapies but wide 95% confidence intervals leave modest risk changes possible.
The strongest evidence centers on species differences in thyroid biology. Rodent C‑cell findings show calcitonin release and neoplasia with receptor stimulation. Human trials up to 52 weeks including obesity doses of liraglutide to 3 mg did not demonstrate systematic calcitonin increases.
Key uncertainties stem from long timelines for tumor development. Pancreatic carcinogenesis can take roughly 12 years from initiation to diagnosis, so current trial and observational follow-up may miss rare or delayed signals.
- Evidence strong species-specific thyroid effects and short-term metabolic benefits.
- Evidence limited very long term cancer outcomes and small changes in rare event rates.
- Practical guidance weigh cardiometabolic gains screen for contraindications history of pancreatitis MEN2 start low and titrate, and document shared decision-making.
Defining GLP-1 Receptor Agonists and Related Therapies
This section defines the class, how it works, and why choice of agent matters in clinical care.
From exenatide and liraglutide to semaglutide and tirzepatide
Incretin-based receptor agonists include short-acting injectables such as exenatide and lixisenatide and long acting options like liraglutide semaglutide, and dulaglutide.
Tirzepatide is a dual GIP/GLP-1 receptor agonist with potent weight and glucose effects. Some agents are weekly injections; one formulation is oral. These differences influence adherence and drug administration choices.
Mechanisms: incretin biology insulin release and gastric emptying
These medications increase glucose-dependent insulin secretion and lower glucagon. They also suppress hepatic gluconeogenesis and slow gastric emptying.
Central receptor effects reduce appetite and support weight loss. Together these mechanisms explain improvements in glycemia for type 2 diabetes and substantial weight changes seen in trials.
- Indications: multiple agents are FDA-approved for type 2 diabetes; some are approved for chronic weight management.
- Adverse effects: nausea diarrhea vomiting, and constipation are common; labeled warnings include pancreatitis and thyroid tumor risk in select populations.
- Clinical fit: these therapies complement metformin SGLT2 inhibitors, and insulin in comprehensive treatment plans.
Search Intent and Reader Guide: How This Trend Report Answers GLP-1 Drugs and Cancer Questions
This article targets U.S. clinicians and patients seeking clear practical answers about therapeutic use and long-term risk.
Purpose: We separate mechanistic hypotheses from outcomes that matter to people. The report synthesizes preclinical work randomized trials controlled observational studies pharmacovigilance system signals, and patient experience to form balanced conclusions.
Use the reading guide to jump to topics you care about: whether pancreatitis could mediate pancreatic cancer thyroid biology differences FAERS strengths and limits, and weight loss benefits in oncology settings.
- Practical relevance: guidance for patients with personal or family cancer history and clinician oversight.
- Controls matter: comparator choice and inclusion criteria shape perceived risk.
- Where answers come from: trials best for causal safety claims; large observational analyses and meta-analyses add power for rare events.
| Source | Strength | Limitation | Typical Question Answered |
|---|---|---|---|
| Preclinical | Mechanism insights | Species gaps | Biologic plausibility |
| Randomized trials | Controlled causality | Short follow-up | Short-term safety |
| Pharmacovigilance | Signal detection | Reporting bias | Rare event alerts |
| Observational studies | Real-world size | Residual confounding | Longer-term associations |
Key acronyms: FAERS, MEN2, MTC, CVOTs. This article provides action oriented insights, monitoring tips, and shared decision making points while noting that past data require ongoing vigilance.
GLP-1 Drugs and Cancer What Epidemiology and Signals Have Suggested
Epidemiologic evidence offers important perspective but cannot alone prove causality for rare, delayed outcomes.
Cancer risk and simple statistical association are not the same. Observational studies can show links, yet confounding by indication, surveillance intensity, and comorbidities common in diabetes and obesity may produce spurious signals.

Cancer risk vs. association framing the evidence
Claims based analyses comparing therapies report pancreatitis odds ratios near one with wide 95% confidence intervals. Those results do not confirm an elevated risk but cannot exclude modest increases.
Time to cancer considerations and exposure windows
Tumor development is slow. Estimates suggest roughly 12 years from initiation another 7 years for metastatic subclones plus about 3 years to clinical diagnosis. Short follow-up therefore misses long latency effects.
- Comparator choice matters: background cancer rates in diabetes complicate attribution.
- Reporting spikes can inflate early perceived signals; large stable datasets give more reliable estimates.
- Harmonized outcomes and longer, adherence-aware follow-up are needed to refine true cancer risk.
Bottom line: Current studies show no consistent increase in cancer incidence, but longer-duration data are essential to settle remaining uncertainty for patients and clinicians.
Pancreatitis as a Potential Mediator of Pancreatic Cancer Risk
Not all pancreatitis leads to the same cancer trajectory; the type and duration of inflammation matter greatly.
Acute versus chronic disease
Acute versus chronic pancreatitis: different trajectories and risks
Acute episodes typically present with abdominal pain, elevated amylase or lipase, and most patients recover without long-term ductal change.
Chronic pancreatitis involves persistent inflammation, fibrosis, and ductal remodeling features associated with roughly a 26-fold higher pancreatic carcinoma risk compared with people without chronic disease.
Claims databases and real world data odds ratios near 1 with wide CIs
Multiple claims based analyses comparing therapies show pancreatitis odds ratios near 1 versus other antidiabetic treatment, but wide 95% confidence intervals limit exclusion of modest risk shifts.
Early case series reported time to onset averaging 34 days range 4–300 with enzyme rises most recovered supporting predominance of acute presentations.
- Clinical relevance progression to cancer is mainly plausible after chronic inflammation, so acute cases carry different implications.
- Confounders hypertriglyceridemia gallstones alcohol, and poor glycemic control modify pancreatitis risk in patients.
- Practical steps titrate slowly, avoid in those with prior chronic pancreatitis, and evaluate persistent pain or sustained enzyme elevations promptly.
Evidence gap: a randomized trial able to exclude a ≥25% risk change would need ~89,000 patient years per arm so ongoing surveillance adjudicated endpoints, and pooled analyses remain essential.
Preclinical and Animal Evidence Pancreas and Thyroid Findings
A wide range of nonclinical studies have mapped how receptor agonists affect thyroid C cells and the exocrine pancreas in rodents.
Thyroid pathway in rodents: In mice and rats, receptor stimulation raises intracellular cAMP in C cells, prompting calcitonin release and progressive C‑cell hyperplasia. Prolonged exposure in some studies led to adenomas and medullary thyroid carcinoma.
Pancreas histology and inflammation
Exocrine pancreas findings vary by model. Some studies report increased ductal cell proliferation, higher Ki67 indices, inflammatory change, and focal fibrosis.
Other transgenic lines did not replicate those ductal abnormalities. In HIP rats, sitagliptin‑linked proliferation reversed with metformin co‑treatment, suggesting medication interactions can alter tissue responses.
Paradoxical signals: exendin‑4 pre‑treatment reduced enzyme rises in induced pancreatitis models raising the hypothesis of context dependent protective effects.
- Translation limits: supratherapeutic dosing and species differences in receptor expression complicate extrapolation to humans.
- Clinical relevance rodent tumor signals justify labeling caution for medullary thyroid tumors even as human C‑cell studies and one year trials show minimal calcitonin release.
Takeaway: Animal data guide surveillance and hypothesis generation but are not definitive predictors of human tumor risk; standardized preclinical endpoints and aligned dosing paradigms are needed.
Human Data on Pancreatic Safety Enzymes Events and Trials
Human clinical evidence focuses on enzyme trends adjudicated events, and pooled trial summaries.
Liraglutide and similar treatments show small, consistent rises in amylase and lipase that usually remain within normal ranges. These shifts rarely coincide with symptoms and alone do not prove pathologic pancreatitis.
Claims-based analyses report similar acute pancreatitis rates for exenatide or sitagliptin versus other glucose‑lowering therapies, with odds ratios near one and wide 95% confidence intervals. Single randomized clinical trials lack the events needed to exclude modest risk changes.
Large cardiovascular outcome trials LEADER, EXSCEL and others add event data, but pooled analyses are needed to raise statistical precision. Adjudication by blinded committees improves event attribution and reduces diagnostic bias.
Modest enzyme elevations without pain typically do not require stopping therapy; persistent pain or rising enzymes warrant prompt evaluation.
Confounders gallstones high triglycerides, alcohol use, and poor glycemic control shape risk. Active surveillance systems such as FDA Sentinel will help refine incidence estimates over years of follow‑up.
- Practical point: continue treatment in asymptomatic patients with mild enzyme changes, but evaluate new abdominal pain or sustained enzyme rises.
- Monitoring: obtain baseline enzymes only when clinically indicated to avoid misleading signals and unnecessary cessation.
- Conclusion: current human data are broadly reassuring for pancreatic safety but not definitive long‑term pooled results and surveillance are essential.
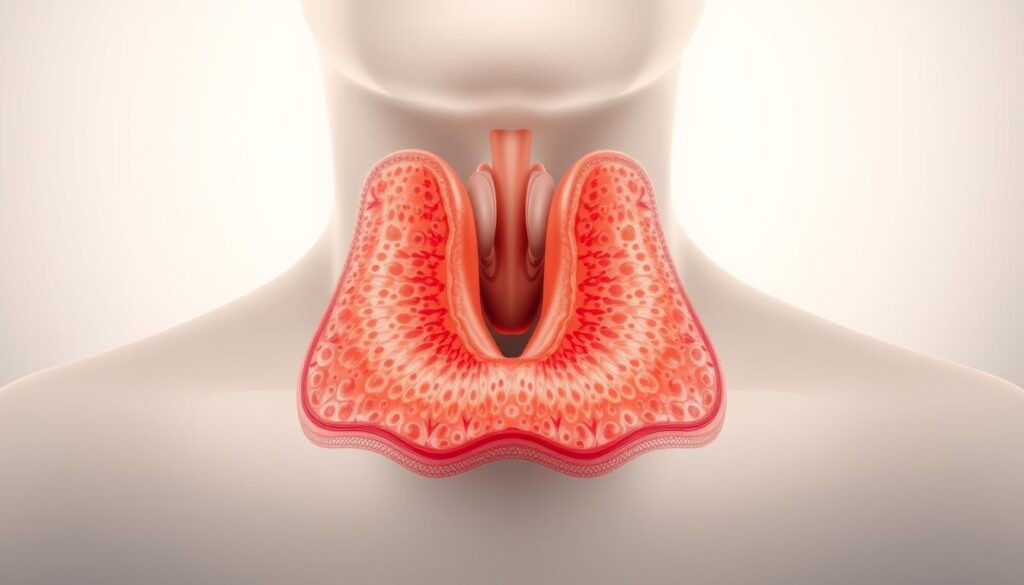
Thyroid Cancer Considerations C-Cell Biology and Medullary Thyroid Signals
Thyroid C cells respond differently across species, which shapes how lab signals translate to people.
Species biology:
Receptor expression and cellular response
Rodent C cells express abundant receptor so stimulation raises cAMP and releases calcitonin. That pathway has produced proliferative lesions and medullary thyroid carcinoma in some animal models.
Human C-cell lines do not show the same cAMP rises or calcitonin secretion at therapeutic exposures. Immunohistochemical findings for receptor presence outside C cells vary across studies and need validation.
Read more: Prostate Cancer Key Facts for Men
Clinical trials labeling and practical guidance
In human trials up to 52 weeks, liraglutide and related agents did not cause sustained calcitonin increases. This trial-level data align with absent evidence of stimulated C-cell proliferation in people to date.
- Labeling caution: avoid receptor agonist use in patients with a personal or family history of medullary thyroid carcinoma or MEN2.
- Monitoring: routine calcitonin screening is not universally recommended but may be reasonable in select high‑risk patients.
- Study design: control comparators and blinded adjudication reduce false signals in trials and registries.
Rodent signals justify caution current human data over available follow-up do not confirm increased thyroid cancer incidence.
| Issue | Animal findings | Human data implication |
|---|---|---|
| Receptor expression | High in rodents | Variable in humans limited functional response |
| Calcitonin response | Marked rise in some studies | No sustained rise in 52‑week trials |
| Regulatory advice | Preclinical caution | Avoid in medullary thyroid carcinoma or MEN2 |
| Clinical action | Hypothesis generation | Assess history shared decision‑making for patients |
What FAERS Can and Cannot Tell Us About Cancer Risk
Spontaneous reporting systems can flag concerns quickly but their raw counts require careful interpretation.
FAERS is designed for signal detection, not incidence estimation. It captures voluntary reports from clinicians, patients, and manufacturers. That makes the system sensitive to underreporting and to sudden surges in submissions.
Between 2004–2009 an analysis found higher reporting odds for pancreatitis (≈11-fold for exenatide, 7-fold for sitagliptin), pancreatic carcinoma (~3-fold), and thyroid carcinoma (4.7-fold for exenatide) versus select antidiabetic comparators. These results raised concern but were controversial.
Reporting bias and stimulated reporting
Media attention legal ads, and regulatory notices can produce waves of reports. This stimulated reporting inflates disproportionality measures temporarily.
Re-analyses and comparator choice
Subsequent studies broadened event definitions and comparator drugs sulfonylureas, metformin, insulin pioglitazone and found different results. Choice of control events and comparator strongly alters reported odds ratios.
FAERS signals should prompt rigorous pharmacoepidemiologic study not immediate causal conclusions.
| Feature | FAERS Finding | Interpretation |
|---|---|---|
| Pancreatitis reports | Elevated odds in early analysis | May reflect reporting bias; needs controlled studies |
| Pancreatic carcinoma | Moderate disproportionality | Short follow-up and aggregation limit inference |
| Thyroid cancer | Higher reporting for one agent | Species signals + reporting spikes; not definitive |
- Takeaway: FAERS helps detect signals but cannot establish causality or true risk.
- Interpret reports alongside controlled studies active surveillance, and trial results before changing practice.
- Improved analytics and linkage to electronic health records will increase the utility of the system.
Obesity Insulin and Estrogen Pathways Why Weight Control Matters in Cancer
Weight status influences key pathways insulin signaling, estrogen production, and inflammation that affect cancer outcomes.
Excess adiposity raises circulating insulin and insulin-like growth factors, which stimulate cell proliferation and may fuel tumor growth. Adipose aromatase converts androgens to estradiol, increasing estrogen exposure after menopause.
Chronic low-grade inflammation from adipocytokines further alters the microenvironment, supporting DNA damage and growth signaling. These mechanisms together create a biologic link between obesity and higher cancer incidence.
Epidemiologic data show that overweight and obese postmenopausal women have higher breast cancer incidence. At diagnosis, obesity correlates with greater recurrence and mortality independent of many comorbidities.
Weight gain during treatment often produces sarcopenic obesity. Muscle loss plus fat gain reduces function, impairs recovery, and can limit tolerance of chemotherapy or radiation.
- Moifiable pathways: improving insulin sensitivity and reducing central fat lower systemic growth signals relevant to disease progression.
- Clinical impacts: weight control can improve surgical outcomes reduce cardiometabolic risk in survivorship, and may favorably change prognosis.
- Intervention note: lifestyle trials show mixed effects on hard oncologic endpoints, but individuals who lose and keep off weight often have better functional and metabolic outcomes.
Combining targeted weight management with high-quality diet and individualized therapy selection offers the best potential to modify pathways that matter for patients.
Practical approach: discuss goals comorbid disease, and readiness for change. Use behavioral strategies plus pharmacologic tools when appropriate to achieve durable weight loss and metabolic benefit.
| Pathway | Effect of Obesity | Clinical implication |
|---|---|---|
| Insulin signaling | Hyperinsulinemia increases mitogenic drive | Improving insulin sensitivity may slow progression |
| Estrogen production | Aromatization in adipose raises estradiol | Higher postmenopausal breast cancer risk |
| Inflammation | Adipocytokines promote pro‑tumor microenvironment | Weight loss and diet quality can reduce inflammation |
| Body composition | Treatment-related weight gain → sarcopenic obesity | Declines function affects therapy tolerance |
GLP-1 RAs in Breast Cancer Context Promise, Evidence Gaps, and Safety
Semaglutide and tirzepatide produced substantial weight loss in trials that excluded breast cancer survivors. That design choice leaves a clear evidence gap for patients and clinicians managing survivorship.
Exclusion of cancer patients from pivotal weight‑loss trials
Registration studies for chronic weight management enrolled adults without recent or active malignancy. Thus, mean weight reductions about 14.9% for semaglutide and 15–21% for tirzepatide do not directly translate to survivor populations.
Current reviews no adverse safety signals identified to date
Systematic reviews and safety summaries have not found breast cancer specific harms linked to these receptor agonists in general populations.
However, oncology cohorts remain underrepresented. Direct evidence on recurrence, progression, and long term outcomes in survivors is sparse.
Preclinical and translational findings
Lab studies show that exendin‑4 reduced proliferation in MCF‑7 and other breast cell lines and slowed growth in mouse models.
One line of work suggests metabolic co‑treatment with metformin may enhance anti‑proliferative signals in tumors.
Weight loss and improved insulin sensitivity may reduce pathways that fuel tumor growth, but direct trial data in survivors are needed.
Practical considerations for survivorship care
- Coordinate care: discuss initiation with the oncology team and review endocrine therapy regimens.
- Monitor tolerability: GI side effects are common; dose titration and nutrition support improve adherence.
- Comprehensive approach: pair medication with resistance exercise, bone health checks, and sarcopenia prevention.
- Data capture: encourage registry enrollment and prospective study participation to record recurrence and safety outcomes.
| Issue | What we know | What is missing |
|---|---|---|
| Trial inclusion | Breast cancer patients excluded | Randomized data in survivors |
| Weight efficacy | ~15–21% mean loss in non‑cancer adults | Effect on recurrence, survival |
| Safety signals | No breast‑specific harms reported | Long‑term oncology outcomes |
Clinical takeaway: For now, discuss potential benefits and unknown risks openly with patients. Individualize treatment decisions align goals for body composition and metabolic health, and update plans as oncology‑specific trial results emerge.
Patient Experience Spotlight Benefits and GI Trade offs
One patient’s journey illustrates how metabolic benefit and new abdominal symptoms can appear together.
Vicki Webb Pouncey, a 58‑year‑old breast cancer survivor, saw minimal change on oral semaglutide (Rybelsus) but large weight loss, lower cholesterol, and improved blood sugar on Wegovy (2.4 mg) and later on Ozempic.
Her gains included reduced insulin resistance and less joint pain. These changes improved daily function and quality of life for this patient.
Common benefits and digestive trade‑offs
Benefits: rapid weight loss, better glycemic indices, and improved labs often meet patient goals.
GI effects: nausea, diarrhea, vomiting, and constipation can escalate with dose or time. Persistent abdominal pain needs prompt evaluation to rule out pancreatitis or other causes.

Read more: Vegan Ketogenic Diet for Cancer
Imaging done for right‑sided pain excluded pancreatitis but found metastatic disease and thyroid nodules pending biopsy.
Vicki emphasizes correlation versus causation and notes thyroid warnings on labels. That nuance matters for informed use.
- Mitigate GI symptoms: slow dose escalation hydration, small low fat meals, antiemetics, temporary dose holds.
- Coordinate care: involve endocrinology or primary care with oncology for shared decisions and monitoring.
- Report symptoms promptly; document patient‑reported outcomes to improve real‑world evidence.
| Feature | Typical benefit | Practical action |
|---|---|---|
| Weight and labs | Marked loss better insulin resistance | Set realistic goals monitor glucose |
| GI side effects | Nausea, diarrhea, vomiting | Slow titration supportive meds |
| Abdominal pain | Rare serious causes | Image promptly exclude pancreatitis |
| Emotional impact | Relief and anxiety when disease is found | Clear counseling multidisciplinary support |
Clinical Trials and Follow up Horizons Why Duration Matters
Large randomized cardiovascular outcome studies provide a rare window into long-term safety, but time limits remain a key weakness when assessing oncologic outcomes.
Cardiovascular outcome trials CVOTs such as LEADER and EXSCEL include adjudicated events and multiple years of follow-up. These trials collect high-quality safety data and allow secondary analyses of pancreatitis and thyroid events in well-characterized cohorts of patients.
However, cancer endpoints are rare and often have long latency. An individual trial, even with several years of follow-up, is unlikely to detect small changes in incidence for new or slow-developing tumors. Meta-analyses that pool trial results improve precision and help address this power gap.
What next generation analyses should include
Consistent case definitions and centralized adjudication are essential to compare results across sponsors and studies. Time-on-drug, cumulative exposure, and latency modeling should be standard parts of safety assessments.
Even pooled trial data may not settle questions for very rare cancers. Real-world evidence, active surveillance systems such as FDA Sentinel, and registries extend follow-up as trials end and drugs reach broader use.
Null findings over limited trial time frames do not fully exclude long-term, small differences in risk; vigilance and standardized reporting matter.
| Asset | Strength | Limitations |
|---|---|---|
| Individual CVOTs | Adjudicated outcomes multi‑year follow‑up | Underpowered for rare long‑latency cancer endpoints |
| Pooled trial meta‑analyses | Better precision harmonized endpoints | Heterogeneity in definitions and exposure time |
| Registries active surveillance | Large size longer time horizons | Potential confounding variable adjudication |
Practical takeaway for clinicians: interpret trial results with attention to follow-up time and exposure. Encourage enrollment in registries, document shared decisions, and use current safety data to guide individualized patient care while monitoring longer-term evidence as it emerges.
Therapy Selection and Risk Mitigation in Practice
Choose therapies using a practical safety checklist that balances metabolic benefit with identifiable patient risks.
Contraindications and thyroid screening
Product labeling advises against use in people with a personal or family history of medullary thyroid carcinoma or MEN2.
Ask about thyroid tumors and familial syndromes before starting treatment. Document the history in the chart and discuss alternatives when contraindications exist.
Managing GI effects and pancreatitis risk
Start low, go slow titrate doses to limit nausea and vomiting. Use dietary measures, temporary dose holds, and symptom-directed medications to preserve adherence.
Assess pancreatitis risk factors up front: triglycerides, gallbladder disease, alcohol use, and uncontrolled diabetes. Investigate persistent abdominal pain or rising enzymes promptly.
- Medication reconciliation: remove overlapping GI‑toxic agents when possible.
- Follow-up checklist: symptoms review, weight trend, targeted labs as indicated, and reassessment of contraindications.
- Alternatives: behavioral programs, other anti‑obesity options, or bariatric referral when use is contraindicated or poorly tolerated.
- Equity note: address access, affordability, and prior‑authorization barriers to support sustained control and adherence.
| Action | What to do | When |
|---|---|---|
| Thyroid history | Screen for medullary thyroid carcinoma/MEN2; document family history | Before initiation |
| GI management | Slow titration, dietary counseling, hold dose if severe | During titration and routine visits |
| Pancreatitis risk | Check triglycerides, review gallbladder history, counsel on alcohol | Baseline and as clinically indicated |
| Follow-up | Use visit checklist; review goals, labs, and tolerability | Every 1–3 months initially, then periodic |
Research Priorities From Mechanisms to Long term Outcomes
Priority studies should link tissue biology to prolonged safety monitoring in real-world patients.
Clear, harmonized research will resolve whether early signals translate into meaningful long-term risk.
Standardizing endpoints for pancreatitis and thyroid neoplasms
First, create agreed definitions that separate acute from chronic pancreatitis and specify thyroid neoplasm staging. Standardized, adjudicated endpoints make pooled analyses valid across sponsors and investigators.
Inclusion of oncology populations in future studies
Design clinical trials that enroll cancer survivors and active oncology patients. Capture recurrence, progression, and quality-of-life outcomes while documenting exposure time and cumulative dose over years.
- Biomarkers: serial calcitonin, structured thyroid ultrasound, inflammatory markers to catch early signals without excess false positives.
- Mechanistic work: human tissue studies to reconcile rodent C‑cell findings with human receptor biology and downstream signaling.
- Surveillance: long-term registries and active platforms to link EHRs with claims for robust follow-up.
Transparent methods, collaboration across endocrinology, oncology, epidemiology, and open data sharing will be essential.
Conclusion
Conclusion
Overall, current human studies provide reassurance while highlighting the need for longer follow-up. strong, The balance of evidence does not establish a higher cancer incidence in treated patients though rodent receptor findings justify caution for those at high risk.
Observational analyses show pancreatitis rates near comparators with wide confidence intervals. Rare events and long latency mean multi‑year surveillance, registries, and pooled trials remain essential.
Clinical takeaway: individualize treatment, follow contraindications for medullary thyroid disease and MEN2, monitor tolerability, and coordinate care for survivors. Encourage shared decision‑making and support participation in long‑term studies to sharpen risk estimates over time.





