Can the trillions of microorganisms in your gut really influence your mood, cognitive function and overall health?
Recent studies have shed light on the complex relationship between the gut microbiome and the brain, revealing a bidirectional communication network known as the gut brain axis.
This intricate system plays a crucial role in regulating various physiological processes, including immune function and the production of certain neurotransmitters. Dysbiosis, or an imbalance in the gut bacteria, has been linked to various disorders, including depression and anxiety.
This article will explore the current scientific understanding of the gut-brain axis and discuss the role of dietary interventions in maintaining a healthy gut microbiome.
Key Takeaways
- The gut microbiome plays a crucial role in overall health and wellness.
- The gut-brain axis is a bidirectional communication network between the gut and the brain.
- Dysbiosis has been linked to various mental health disorders, including depression.
- Dietary interventions can help maintain a healthy gut microbiome.
- Understanding the gut-brain axis can lead to new approaches in treating mental and physical health conditions.
Understanding the Gut Microbiome
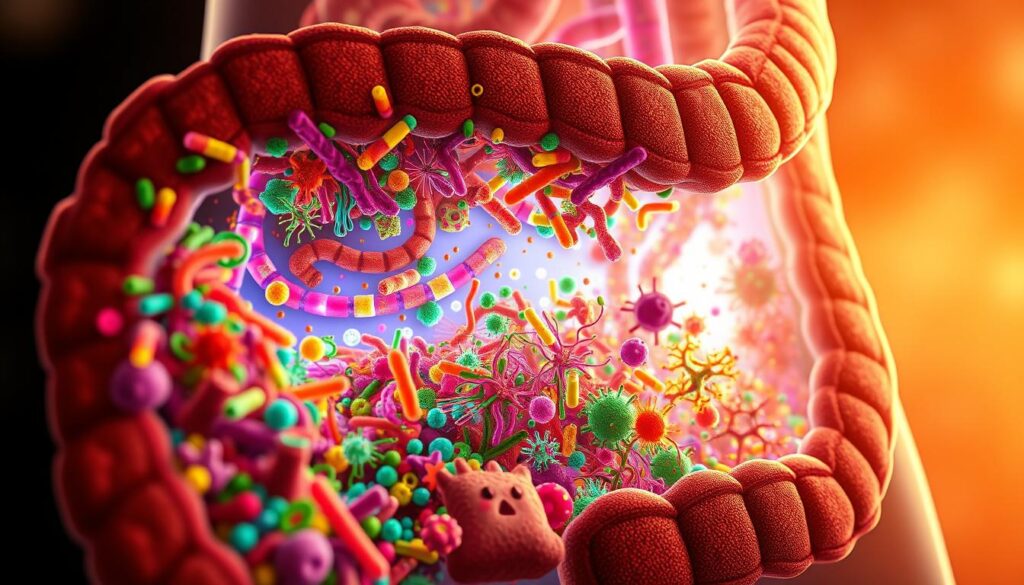
The gut microbiome, comprising various microorganisms, is a vital component of our bodily health. It is primarily located in the large intestine, where it plays a crucial role in our overall well-being.
What Is the Gut Microbiome?
The gut microbiome refers to the complex community of microorganisms residing mainly in the large intestine. These microbes include bacteria viruses fungi, and other microscopic living things collectively known as the microbiome.
The human body contains more bacterial cells than human cells, with approximately 40 trillion bacterial cells compared to 30 trillion human cells. This remarkable fact highlights the significance of the gut microbiome in our bodily functions.
The Composition of a Healthy Microbiome
A healthy microbiome is characterized by its diversity and balance. The gut microbiome consists of various microbial species with Bacteroidetes and Firmicutes being the predominant bacterial phyla. These microbes contribute to the maintenance of homeostasis, or balance, within the body which is essential for overall health.
| Microbial Species | Function |
|---|---|
| Bacteroidetes | Carbohydrate metabolism |
| Firmicutes | Energy extraction and storage |
The concept of enterotypes, which classify human gut microbiomes into distinct types based on dominant bacterial species further emphasizes the individuality of microbiome compositions. Understanding the composition of a healthy microbiome is crucial for appreciating its role in our overall health and well-being.
The Development of Our Gut Microbiome
The journey of gut microbiome development begins prenatally and is shaped by numerous factors throughout an individual’s lifespan. Research has shown that the initial colonization of the microbiome occurs even before birth, with the placenta and amniotic fluid playing a crucial role in this process.
Factors Affecting Initial Microbiome Formation
The formation of the gut microbiome is influenced by several factors from the moment of conception.
Studies have indicated that maternal stress during pregnancy can affect the fetal microbiome with decreased levels of beneficial bacteria such as Bifidobacterium observed in animal studies. The mode of delivery also significantly impacts the initial microbiome composition with vaginally delivered infants having a more diverse gut microbiota compared to those born via Cesarean section.
From Infancy to Adulthood: How Our Microbiome Evolves
As we grow from infancy through adulthood, our gut microbiome continues to evolve. The introduction of solid foods during infancy represents a critical period in microbiome development leading to increased diversity and functionality.
Throughout childhood and adolescence, the microbiome continues to adapt to dietary changes and environmental exposures, eventually stabilizing in adulthood. However it remains responsive to various factors including diet and lifestyle choices.
The Role of Diet in Microbiome Development
Diet plays a crucial role in shaping the gut microbiome throughout life. Breast milk, for instance, provides oligosaccharides that nourish beneficial bacteria like Bifidobacterium, promoting a healthy infant microbiome.
As we transition to solid foods, a diverse diet rich in fiber supports the growth of a wide range of beneficial microbial species. This dietary influence on the microbiome continues into adulthood, with ongoing studies examining the impact of different dietary patterns on gut health.
The Gut Microbiome A Key Factor in Mental and Physical Health
The intricate relationship between the gut microbiome and overall health is becoming increasingly evident, with research highlighting its crucial role in both mental and physical well-being. The gut microbiome is not just a collection of microorganisms living in the digestive tract it’s a complex ecosystem that influences various aspects of health.
The Gut Brain Axis Explained
The gut-brain axis is a bidirectional communication network that integrates gut functions with the brain’s cognitive and emotional centers.
This complex system involves the central nervous system the autonomic and enteric nervous systems as well as the neuroendocrine enteroendocrine, and neuroimmune systems. The vagus nerve serves as a direct communication highway between the gut and brain transmitting signals that influence mood cognition, and stress responses.
The gut-brain axis plays a crucial role in mediating the effects of genetic and environmental factors on brain development and function. Research has associated this axis with the etiology of several psychiatric disorders highlighting the importance of the gut microbiome in mental health.
How Gut Bacteria Influence Overall Health
Gut bacteria produce neurotransmitters like serotonin, GABA, and dopamine that can affect brain function and mental states. Notably, approximately 90% of serotonin is produced in the gut. Microbial metabolites, including short-chain fatty acids, influence systemic health by regulating inflammation, metabolism, and immune function.
Emerging research shows correlations between gut microbiome composition and various health conditions, from mental health disorders to metabolic diseases. The gut microbiome’s effects extend beyond digestion to influence virtually every system in the body, highlighting its role as a central regulator of health.
Understanding the gut microbiome’s influence on overall health can lead to new approaches in preventing and treating a range of diseases. By focusing on maintaining a healthy gut microbiome, individuals can potentially improve their mental and physical well-being.
Gut Dysbiosis When the Microbiome Balance Is Disrupted
Disruption in the gut microbiome, or dysbiosis, can have significant implications for both mental and physical well-being. The gut microbiome plays a crucial role in maintaining overall health, and its imbalance can lead to various health issues.
Causes of Gut Dysbiosis
Several factors can contribute to the development of gut dysbiosis. These include a poor diet, especially one high in processed foods and sugar, chronic stress, antibiotic use, lack of sleep, and exposure to environmental toxins. Such factors can disrupt the delicate balance of the gut microbiome, leading to dysbiosis.
The impact of these factors can be seen in the way they alter the composition of the gut microbiome. For instance, a diet lacking in fiber can reduce the population of beneficial bacteria, while antibiotic use can indiscriminately kill both harmful and beneficial bacteria, leading to an imbalance.
Signs and Symptoms of an Unhealthy Gut
Recognizing the symptoms of gut dysbiosis is crucial for early intervention. Common signs include digestive issues such as bloating, gas, diarrhea, and constipation. Additionally individuals may experience food intolerances fatigue, skin problems autoimmune conditions, and mood disorders.
These symptoms can be indicative of an underlying issue with the gut microbiome. For example increased intestinal permeability often referred to as leaky gut syndrome can allow bacterial metabolites and inflammatory molecules to enter the bloodstream contributing to chronic inflammation and potentially leading to various diseases.

The relationship between gut dysbiosis and overall health is complex. Chronic inflammation resulting from dysbiosis can affect multiple body systems creating a cycle of worsening health outcomes. Certain bacterial populations may become overrepresented in a dysbiotic gut while beneficial species decline further disrupting the balance necessary for optimal health.
| Common Causes | Signs and Symptoms | Health Implications |
|---|---|---|
| Poor diet | Digestive issues | Chronic inflammation |
| Chronic stress | Food intolerances | Disease development |
| Antibiotic use | Fatigue, skin problems | Autoimmune conditions |
Early recognition of the signs of dysbiosis can help prevent more serious health conditions from developing. By understanding the causes and symptoms of gut dysbiosis, individuals can take proactive steps to maintain a healthy gut microbiome.
The Gut Brain Connection: Communication Pathways
The intricate relationship between the gut and brain is maintained through several key communication channels. This complex network enables the constant exchange of information, influencing each other’s functions and overall health.
Neural Pathways The Vagus Nerve
The vagus nerve is the primary neural pathway connecting the gut and brain.
It transmits signals in both directions allowing gut molecules to influence mood and the brain to send signals back to the gut. The enteric nervous system often called the second brain contains over 100 million neurons and can function independently while maintaining communication with the central nervous system.
Immune System Signaling
The immune system serves as a signaling pathway between the gut and brain. Immune cells respond to gut microbes and produce cytokines that can affect brain function. This communication pathway is crucial for maintaining overall health and influencing the effects of the gut-brain axis.
Microbial Metabolites and Neurotransmitters
Gut bacteria produce various neurotransmitters including serotonin dopamine, and GABA that can influence mood and cognition.
Microbial metabolites, particularly short chain fatty acids like butyrate, propionate, and acetate, act as signaling molecules that affect brain function and behavior.
These metabolites can reach the brain through the vagus nerve and the bloodstream, further highlighting the complex communication pathways between the gut and brain.
The communication between the gut and brain is a two-way street, with hormonal pathways including the hypothalamic pituitary adrenal HPA axis connecting gut function with stress responses and emotional regulation. Understanding these pathways is essential for appreciating the intricate relationship between the gut brain, and overall well-being.
- The vagus nerve plays a critical role in the gut brain axis, facilitating bidirectional communication.
- The enteric nervous system can function independently while communicating with the central nervous system.
- Gut bacteria produce neurotransmitters that influence mood and cognition.
- Microbial metabolites act as signaling molecules affecting brain function and behavior.
How Gut Bacteria Influence Mental Health
As research continues to unravel the mysteries of the gut-brain axis, it has become increasingly clear that gut bacteria are pivotal in maintaining mental health. The gut microbiome produces various metabolites that can influence brain function, thereby affecting mood and behavior.
The Microbiome’s Role in Depression and Anxiety
Recent studies have demonstrated characteristic variations in the gut microbiome of individuals with depression and anxiety. Certain bacteria produce neurotransmitters like serotonin and GABA which have a potent neurological action. These substances can exert their effects through the vagus nerve influencing mood and depression.
People with depression and anxiety often have distinct gut microbiome compositions compared to those without these conditions, suggesting a biological connection between the gut and mental health.
Stress Response and the HPA Axis
The gut microbiome helps regulate the body’s stress response through the hypothalamic-pituitary adrenal HPA axis.
Dysregulation of this system is a hallmark of depression and anxiety disorders. Studies have shown that germ-free mice exhibit an exaggerated response to stressors, indicating that the presence of microbiota may moderate the stress response.
Inflammation and Mood Disorders
Chronic inflammation often stemming from gut dysbiosis, contributes to the development and persistence of mood disorders through inflammatory cytokines that affect brain function. This highlights the importance of maintaining a balanced gut microbiome for overall mental health.
By understanding the intricate relationship between gut bacteria and mental health, we can explore new avenues for treating depression and anxiety, potentially leading to improved mental wellness outcomes.
The Microbiome’s Impact on Cognitive Function
The intricate relationship between the gut microbiome and cognitive function is becoming increasingly evident. Research has shown that the gut microbiome influences various cognitive processes including memory, concentration, and overall brain development.
Gut Health and Brain Development
The development of the brain is a complex process that is influenced by the gut microbiome, particularly during critical periods such as prenatal development childhood, and adolescence.
Microbial metabolites including short chain fatty acids like butyrate play a crucial role in this process by crossing the blood-brain barrier and affecting neuroplasticity and neurogenesis.
Studies have demonstrated that the composition of the gut microbiome is correlated with cognitive performance. For instance, probiotic supplementation has been shown to improve certain cognitive functions, highlighting the potential for microbiome-based interventions to support brain health.
Microbiome Influence on Memory and Concentration
The gut microbiome influences the production of brain-derived neurotrophic factor BDNF a protein crucial for neural development and cognitive function.
Additionally the integrity of the blood-brain barrier, which protects the brain from harmful substances, is affected by the gut microbiome.
Emerging research suggests that the gut microbiome may play a role in neurodegenerative conditions and cognitive decline. Understanding this relationship could lead to preventive strategies that support cognitive health through the modulation of the gut microbiome.
| Cognitive Function | Gut Microbiome Influence |
|---|---|
| Memory | Microbial metabolites affect neuroplasticity |
| Concentration | Probiotic supplementation improves cognitive performance |
| Brain Development | BDNF production influenced by gut bacteria |
As research continues to uncover the mechanisms by which the gut microbiome influences cognitive function, it becomes clear that maintaining a healthy gut microbiome is essential for overall brain health.
Gut Health and the Immune System
The intricate relationship between the gut microbiome and the immune system is vital for our well being. Approximately 70-80% of our immune cells reside in the gut associated lymphoid tissue GALT underscoring the significance of gut health in immune function.
How Gut Bacteria Train Our Immune Response
Gut bacteria play a crucial role in training our immune system from birth, helping it distinguish between harmful pathogens and beneficial or harmless substances.
Commensal bacteria in the gut maintain the intestinal barrier preventing leaky gut syndrome and the systemic inflammation that can result from increased intestinal permeability.
Short chain fatty acids produced by gut bacteria regulate immune cell function and development influencing both innate and adaptive immune responses.
As noted by a study In patients with inflammatory bowel disease probiotics correlated with suppressed levels of pro-inflammatory cytokines, and improved intestinal barrier integrity. This highlights the potential of beneficial bacteria in modulating the immune response and reducing inflammation.
| Mechanism | Effect on Immune System |
|---|---|
| Gut bacteria training immune cells | Distinguishes between harmful and harmless substances |
| Maintaining intestinal barrier integrity | Prevents leaky gut syndrome and systemic inflammation |
| Production of short-chain fatty acids | Regulates immune cell function and development |
Autoimmune Conditions and the Microbiome
Gut dysbiosis has been linked to various autoimmune conditions, including inflammatory bowel disease rheumatoid arthritis multiple sclerosis, and type 1 diabetes.
Certain bacterial species can either promote or suppress inflammation, highlighting the importance of microbial balance for proper immune function. Early life microbiome development influences immune system programming and may affect susceptibility to allergies and autoimmune conditions later in life.
The connection between gut health and autoimmune diseases is complex and multifaceted, involving the interplay of genetic environmental, and microbial factors. Understanding this relationship is crucial for developing effective prevention and treatment strategies.
The gut microbiome is a key factor in the development and function of the immune system, and alterations in the microbiome have been linked to various diseases, including autoimmune disorders.
The Gut Microbiome and Digestive Health
The gut microbiome plays a crucial role in maintaining digestive health. A balanced gut microbiome is essential for proper digestive function, and its imbalance can lead to various gastrointestinal disorders.
The concept of microbial diversity is a key indicator of digestive health. Studies have shown that individuals with a higher diversity of gut microbiota, often referred to as having a high gene count HGC have better digestive function and a reduced risk of metabolic diseases and obesity.
Irritable Bowel Syndrome and the Microbiome
Irritable Bowel Syndrome IBS is a common gastrointestinal disorder characterized by symptoms such as bloating, abdominal pain, and altered bowel habits. Research has shown that dysbiosis or an imbalance in the gut microbiome contributes to the development of IBS symptoms.
- Increased Firmicutes to Bacteroidetes ratio
- Decreased abundance of beneficial bacteria like Bifidobacteria
- Altered gut motility and gas production
Inflammatory Bowel Disease: The Microbiome Connection
Inflammatory Bowel Disease IBD which includes conditions such as Crohn’s disease and ulcerative colitis, is associated with an imbalance in the gut microbiome. Certain bacterial species can either promote or protect against intestinal inflammation.
Emerging therapeutic approaches targeting the microbiome for digestive disorders include:
- Fecal microbiota transplantation
- Prebiotics and probiotics
- Dietary interventions aimed at promoting a balanced gut microbiome
By understanding the role of the gut microbiome in digestive health and disease, we can develop effective strategies to prevent and treat gastrointestinal disorders.
The Microbiome’s Role in Weight Management
Research has shown that the gut microbiome influences metabolism and weight regulation. The human gut is home to thousands of different types of bacteria, most of which are beneficial to our health. However, an imbalance between healthy and unhealthy microbes, known as gut dysbiosis, can lead to various health issues including weight gain.
Studies involving identical twins, where one twin had obesity and the other did not have provided valuable insights into the role of the microbiome in weight management. These studies demonstrated that the gut microbiome differed significantly between the twins indicating that the differences were not genetic.
When the microbiome from the twin with obesity was transferred to mice, they gained more weight than those that received the microbiome from the lean twin, despite both groups consuming the same diet.
How Gut Bacteria Affect Metabolism
Gut bacteria play a crucial role in metabolism by influencing energy extraction from food regulating fat storage and affecting appetite regulating hormones.
Certain bacterial populations can extract different amounts of energy from the same foods potentially contributing to weight gain or loss independent of caloric intake. This mechanism highlights the complex relationship between the gut microbiome and metabolism.
Microbiome Differences in Obesity
The composition of the microbiome varies significantly between lean individuals and those with obesity.
Typically, there are shifts in the ratio of major bacterial phyla, such as Firmicutes and Bacteroidetes. These differences can influence insulin sensitivity and glucose metabolism, affecting the risk factors for metabolic syndrome and type 2 diabetes.
Dietary changes can shift the microbiome composition toward patterns associated with healthier weight management, potentially offering new approaches to addressing obesity. By understanding the role of the gut microbiome in weight regulation, we can explore novel therapeutic strategies to manage weight and related metabolic disorders.
The Gut Microbiome and Heart Health
Recent studies have uncovered a fascinating relationship between the gut microbiome and heart disease risk. The gut microbiome plays a crucial role in maintaining heart health by influencing various factors associated with cardiovascular well-being.
Bacterial Metabolites and Cardiovascular Risk
Certain bacteria within the gut microbiome metabolize dietary components to produce trimethylamine N-oxide TMAO a compound associated with an increased risk of atherosclerosis and heart disease.
TMAO is produced when bacteria convert choline and L-carnitine, nutrients found in red meat and other animal-based food sources. Increased TMAO levels have been linked to a higher risk of heart attacks and strokes.
| Dietary Component | Bacterial Metabolite | Cardiovascular Risk |
|---|---|---|
| Choline, L-carnitine | TMAO | Increased risk of atherosclerosis |
| Plant-based fibers | Short-chain fatty acids | Reduced inflammation, improved heart health |
Cholesterol Regulation and Gut Bacteria
Beneficial gut bacteria can help regulate cholesterol levels by breaking down bile acids and preventing cholesterol reabsorption in the intestines.
Certain probiotic strains particularly Lactobacilli, have been shown to reduce LDL cholesterol levels and improve other cardiovascular risk markers. A healthy gut microbiome supports overall heart health by maintaining a balance between different bacterial species.
By understanding the intricate relationship between the gut microbiome and heart health, individuals can make informed dietary choices to support cardiovascular well-being. Incorporating a balanced diet rich in plant-based foods and maintaining a healthy gut microbiome can contribute to reduced heart disease risk.
Microbiome’s Influence on Blood Sugar and Diabetes Risk
The gut microbiome plays a crucial role in controlling blood sugar levels, which can significantly impact the risk of developing type 1 and type 2 diabetes. Recent studies have shed light on the intricate relationship between the gut microbiome and glucose metabolism.

The gut microbiome influences glucose metabolism and insulin sensitivity through various mechanisms. Certain gut bacteria produce metabolites that either enhance or impair the body’s response to insulin.
For instance, short-chain fatty acids produced by beneficial gut bacteria help regulate blood sugar levels by improving insulin secretion and sensitivity.
Gut Bacteria and Insulin Sensitivity
Gut bacteria play a significant role in modulating insulin sensitivity. Research has shown that specific strains of gut bacteria can improve insulin sensitivity by producing anti-inflammatory metabolites. Conversely, an imbalance in the gut microbiome also known as dysbiosis, can lead to decreased insulin sensitivity and an increased risk of developing type 2 diabetes.
Studies have demonstrated that the diversity of the gut microbiome is often reduced in individuals with diabetes. This reduction in microbiome diversity can lead to a decrease in beneficial bacteria that produce short-chain fatty acids, further impairing insulin sensitivity.
Microbiome Patterns in Type 1 and Type 2 Diabetes
Research has identified distinct microbiome patterns in individuals with type 1 and type 2 diabetes. In type 1 diabetes, a sudden drop in microbiome diversity often precedes the onset of the disease. In contrast, type 2 diabetes is characterized by decreased butyrate-producing bacteria and increased opportunistic pathogens.
Understanding these microbiome patterns can provide valuable insights into the development of diabetes and potentially lead to novel therapeutic strategies. For instance, targeting specific gut bacteria or using probiotics to modulate the gut microbiome may offer new avenues for diabetes prevention and management.
Dietary Strategies to Improve Gut Health
Adopting a diet rich in diverse foods is crucial for maintaining a healthy gut microbiome. A diverse diet can lead to a diverse microbiome, which is an indicator of good gut health. In particular, legumes, beans, and fruits contain lots of fiber and can promote the growth of healthy Bifidobacteria.
Fiber-Rich Foods and Prebiotics
Dietary fiber plays a critical role in feeding beneficial gut bacteria. Different types of fiber, such as soluble insoluble, and resistant starch, support various bacterial populations. Prebiotic-rich foods include artichokes, bananas, asparagus, oats, and apples. These foods contain specialized fibers that selectively nourish beneficial bacteria.
| Prebiotic Food | Beneficial Effect |
|---|---|
| Artichokes | Nourishes beneficial bacteria |
| Bananas | Promotes growth of healthy Bifidobacteria |
| Asparagus | Supports diverse gut microbiome |
Fermented Foods and Their Benefits
Fermented foods like yogurt, kefir, sauerkraut, kimchi, and kombucha contain live beneficial bacteria that can temporarily colonize the gut and provide health benefits. These foods can reduce the amount of disease-causing species in the gut.
The consumption of fermented foods is a practical dietary strategy for promoting a healthy gut microbiome.
Foods to Limit for Optimal Gut Health
To maintain optimal gut health, it’s essential to limit the intake of certain foods and substances that may harm gut microbiome diversity. These include highly processed foods artificial sweeteners excessive alcohol, and certain emulsifiers and additives. Limiting these can help support a diverse and healthy microbiome.
- Highly processed foods
- Artificial sweeteners
- Excessive alcohol
- Certain emulsifiers and additives
Eating a diverse range of foods and being mindful of dietary choices can significantly improve gut health. By incorporating fiber-rich foods, fermented foods, and limiting harmful substances, individuals can promote a healthy gut microbiome and overall health.
The Role of Probiotics in Mental and Physical Wellness
Recent research highlights the role of probiotics in supporting both mental and physical well-being. Probiotics are live microorganisms that confer health benefits when consumed in adequate amounts. They have been utilized as supplements to other medications or as alternative treatments for anxiety and depression.
Types of Beneficial Probiotics
Probiotics include various genera, with Lactobacillus and Bifidobacterium being key strains that have shown mental health benefits. These beneficial bacteria can influence mental health through multiple mechanisms including reducing inflammation, modulating stress hormones, and producing neuroactive compounds.
The specific strains of probiotics can have different effects on the body. For instance, certain strains have been shown to improve symptoms of depression and anxiety. Understanding the different types of probiotics and their benefits is crucial for selecting the right supplement.
Research on Probiotics for Depression and Anxiety
Clinical studies have demonstrated that certain probiotic strains can reduce symptoms of depression and anxiety.
In some cases, the effectiveness of probiotics has been comparable to conventional medications. For example, a 30-day study found that healthy volunteers given probiotics showed reduced cortisol levels and improved self-reported psychological effects, similar to those administered Diazepam.
Probiotics can influence mental health by reducing inflammation and modulating stress hormones. The concept of psychobiotics refers to probiotics specifically selected for their mental health benefits. Emerging research in this field is promising suggesting that probiotics could be a valuable tool in managing mental health conditions.
When selecting probiotic supplements, considerations include strain specificity, colony-forming units CFUs, and product stability. Ensuring that the probiotics are of high quality is essential for achieving the desired health benefits.
Lifestyle Factors That Impact the Gut Microbiome
Our daily habits and lifestyle decisions have a profound impact on the balance and diversity of our gut microbiome. While diet is a well-known factor, other aspects of our lifestyle also play a crucial role in shaping the health of our gut.
The Impact of Physical Activity
Regular exercise and physical activity are known to promote microbiome diversity and the growth of beneficial bacterial populations. This can occur through several mechanisms, including altered transit time, reduced inflammation, and improved metabolism, all of which contribute to a healthier gut.
Sleep Quality and the Microbiome
The relationship between sleep and the gut microbiome is bidirectional. Poor sleep can disrupt the microbial balance, while the health of the gut microbiome can influence sleep quality through the production of melatonin and other sleep regulating compounds. Ensuring good sleep hygiene is essential for maintaining a healthy gut.
Managing Stress for Gut Health
Chronic psychological stress can negatively affect the gut microbiome by increasing intestinal permeability, altering bacterial composition, and promoting inflammation. Practicing stress management techniques such as mindfulness meditation, deep breathing exercises, yoga, and spending time in nature can support gut health.
Addressing multiple lifestyle factors simultaneously is crucial for optimal gut microbiome health, as these factors often work synergistically. By making informed choices about our lifestyle, we can positively influence the composition and function of our gut microbiome, leading to improved overall health.
Conclusion Nurturing Your Microbiome for Overall Wellness
As we conclude our exploration of the gut microbiome, it’s clear that nurturing this complex ecosystem is crucial for overall wellness. Throughout this article, we’ve delved into the intricate relationships between the gut, brain, and overall health, highlighting the bidirectional nature of the gut-brain axis.
The significance of maintaining a balanced microbiome cannot be overstated, as it influences not only mental health but also physical health, impacting aspects such as mood, cognition, immunity, and metabolism. To support a healthy gut, it’s recommended to consume a diverse diet rich in fruits vegetables whole grains, and fermented foods.
Adopting a plant-based diet and incorporating foods high in polyphenols, such as those found in red wine, green tea, and dark chocolate, can stimulate healthy bacterial growth. Additionally, considering probiotic supplements and limiting antibiotics to only when medically necessary can further support gut health.
It’s essential to recognize that gut health is highly personalized, and responses to interventions may vary. Thus, paying attention to your body’s signals and making informed dietary choices is key. By making small, consistent changes to support your microbiome, you can potentially achieve significant improvements in your overall quality of life.
In conclusion, nurturing your gut microbiome is a proactive step towards achieving better health and wellness. As research continues to evolve, the importance of this complex ecosystem will only continue to grow, underscoring the need for a holistic approach to health that includes supporting your gut.





