Can tiny residents inside your body shape the way you feel? This guide asks that question up front to unsettle assumptions and spark curiosity.
This article pulls together recent study findings on the microbiome-gut brain axis. It explains how the gut microbiota links to disorders such as anxiety and depression, and it highlights patterns seen in human samples and animal models.
The narrative covers composition, mechanisms like the HPA axis and vagus nerve, key metabolites such as SCFAs, and practical notes on probiotics and fecal transplant trials. Evidence ranges from association studies to causal clues in rodents with clinical trials still limited.
Expect a clear, evidence-focused article that points readers in the right direction for further reading on google scholar and for discussions with clinicians in the United States.
Key Takeaways
- Current studies link microbiota shifts to symptoms across several disorders.
- Mechanisms include metabolites, immune signals, and neural pathways.
- Animal work gives causal hints human trials are promising but limited.
- Probiotics and FMT show variable effects use as adjuncts, not replacements.
- Use google scholar to review primary research and verify clinical claims.
Why the Gut-Brain Connection Matters for Mental Health
The digestive tract communicates with the central nervous system through a web of neural, immune, endocrine, and metabolic signals. This bidirectional network links gut microbiota to circuits that regulate mood, stress, and cognition. Animal models show germ-free status changes stress responses, BDNF levels, and vagus-driven signaling.
Clinical relevance: Human observational work finds altered microbiota and lower diversity in anxiety and depression. Small intervention trials diet shifts, probiotics, and FMT report symptom improvements for some people, though results vary.
The axis is not a single route. Coordinated signals include cytokines, cortisol via the HPA axis, and vagal activity. Disrupted barrier function and inflammation can worsen symptoms across multiple disorders.
- Function often matters more than exact composition different communities can produce similar metabolites.
- Early modulation diet, targeted strains may complement standard care.
- Readers can use google scholar to review larger cohorts and replication studies.
Defining the Microbiome Microbiota and the Microbiota Gut Brain Axis
This section explains core terms and the main routes that connect intestinal life to the nervous system.
Microbiome refers to all microorganisms plus their genes. Microbiota names the organisms in a body site, such as the gut. The microbiota gut brain axis is the integrated network linking those organisms to brain function.
Key communication pathways
- Neural: vagus nerve and enteric circuits carry fast signals.
- Endocrine: stress hormones via the hpa axis alter cortisol rhythms.
- Immune: cytokines change barrier permeability and signaling to the brain.
From correlation to causation
FMT experiments in mice receiving stool from depressed or anxious donors produce parallel behavior changes. These transfers implicate tryptophan metabolism immune shifts and oxytocin system changes.
Species-level roles differ, so microbiota composition should be paired with functional assays. For primary reports and mechanistic reviews use google scholar to locate foundational studies and reproducible evidence cited in this article.
How Microbiota Develop from Birth to Adulthood
Early life events set a lasting course for the developing intestinal community and its interactions with the body. Vertical transmission begins before birth, and delivery mode shapes initial colonization: vaginal birth usually yields higher early bacterial loads than Cesarean delivery.

Birth mode, breastfeeding, and early diet shape microbiota composition
Breastfeeding raises Bifidobacterium levels, supplies IgA, and tends to lower IL-6 compared with formula. Human milk oligosaccharides selectively feed protective species during a critical window.
Weaning and introduction of solid food drive a shift toward adult-dominant Bacteroidetes and Firmicutes. Short term dietary changes cause rapid composition shifts, but many profiles rebound once habitual intake resumes.
Enterotypes diversity and functional redundancy in the adult gut
Adult enterotypes Bacteroides, Prevotella, Ruminococcus often reflect habitual macronutrient patterns more than geography or age.
Diversity matters: higher richness supports vitamin synthesis immune tolerance, and SCFA production. Functional redundancy means different taxonomic arrays can preserve similar metabolic roles if diversity remains adequate.
- Perinatal factors measurably affect early microbiota composition and immune levels.
- Dietary choices across childhood steer long term community structure.
- For primary reports search google scholar to review cohort and mechanistic study data.
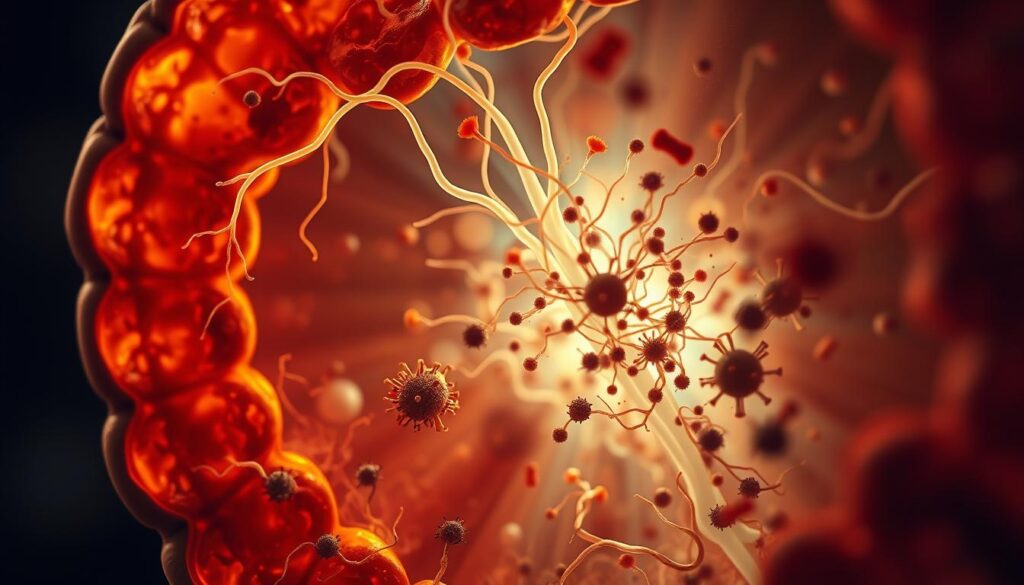
Core Mechanisms Linking Gut and Brain
Signals from the intestinal environment shape stress responses barrier integrity, and neurotransmitter balance through several interacting mechanisms.
HPA axis activation, cortisol and stress reactivity
Stress triggers the hpa axis, raising cortisol levels that alter digestive permeability and immune tone. Dysbiosis can heighten stress reactivity, forming a feedback loop that affects mood and cognition.
Vagus nerve signaling and BDNF driven neuroplasticity
Microbial signals influence BDNF and synaptic plasticity via vagal routes. Vagotomy experiments show some probiotic benefits depend on intact vagal signaling, linking intestinal signals to neural change.
Immune pathways cytokines, and leaky gut
Dysbiosis raises intestinal permeability, allowing bacterial products to provoke systemic inflammation. Cytokines such as IL-6 and TNF-α can increase blood brain barrier permeability and correlate with depressive and anxiety symptoms.
Metabolites: short-chain fatty acids, tryptophan pathways, neurotransmitters
SCFAs support barrier integrity and immune regulation, while tryptophan-kynurenine shifts affect serotonin availability. Certain psychobiotic strains modulate dopamine and noradrenaline, showing how metabolites alter neurochemistry.
- These mechanisms are interlinked: immune activation can drive hpa changes, and metabolites can act directly on neural circuits.
- Function and metabolite levels often matter more than which taxa are present.
- Preclinical models provide the strongest mechanistic evidence human multiomics studies in this article point to similar routes search google scholar to locate primary reports.
Translational role: targeting these pathways shapes rational dietary and psychobiotic strategies for disorder risk reduction and adjunctive care. Use google scholar to track mechanistic and clinical trials cited in this article.
Gut Microbes and Mental Health
Human research links shifts in intestinal communities with symptoms across anxiety and depression. Multiple cohorts report lower diversity altered Firmicutes/Bacteroidetes ratios, and fewer SCFA producers in affected people.
Why this matters: loss of beneficial taxa can weaken barrier function and tilt immune balance. That shift may raise systemic inflammation and change signaling to the brain via endocrine neural, and metabolic routes.
Animal transfers show causal effects: stool from symptomatic donors can induce parallel behaviors in rodents. Early clinical trials Mediterranean style diets, multistrain psychobiotics, and FMT have produced adjunctive benefits for some patients but results vary by individual and disorder.
- Function often outweighs exact composition: metabolites and signaling outputs drive many effects.
- Converging animal and human evidence supports a role for the microbiome yet larger trials are needed for firm claims.
For critical appraisal, use google scholar to compare study design sample size and mechanistic measures. Integrate gut directed strategies with standard care and clinician guidance rather than using them as replacements.
What the Evidence Says about Anxiety
Several clinical reports now link anxiety symptoms with consistent shifts in intestinal community richness and function.
Human findings
Patterns emerge: people with anxiety often show lower richness and reduced levels of beneficial SCFA-producing species. Cohorts report altered Firmicutes/Bacteroidetes ratios, with some noting higher Bacteroidetes and Fusobacteria in generalized anxiety disorder.
Specific taxa shifts include reduced Faecalibacterium and changes in Lachnospira and other fiber fermenters. These changes affect SCFA levels, barrier integrity, and immune signaling.
Animal evidence
In mice, higher anxiety like behavior links to lower Firmicutes. Fecal transfers from symptomatic donors can induce anxiety phenotypes in recipients, supporting a causal role for community function rather than a single species.
- Human studies are often cross sectional prospective work is limited.
- Variability across cohorts highlights the need to assess microbiota composition alongside function.
Practical note: search google scholar to compare cohort methods and replication. Restoring diversity and SCFA output through diet and targeted adjuncts complements care while mechanistic research continues. Consult google scholar for primary reports and this article’s cited studies.
Depression: Composition Changes Pathways and Transferability
Research in MDD points to consistent reductions in certain beneficial species alongside rises in taxa tied to inflammation.
Microbiota signatures in major depressive disorder
Multiple cohorts report lower Dialister and Coprococcus in people with depression. Other reports show higher Prevotella and Klebsiella, and in some samples increased Firmicutes with reduced Bacteroidetes.
Findings vary by cohort and method, so use google scholar to compare sample size and replication. Interpret composition alongside functional readouts for a fuller view.
Fecal transfers and causality in rodents
Fecal transfers from depressed donors produce anhedonia and anxiety-like behavior in rodents. These transfers also alter host tryptophan metabolism and energy pathways strengthening causal inference between community function and symptoms.
Tryptophan, serotonin pathways, and sex-related notes
Microbial shifts can change tryptophan-kynurenine routing, reducing serotonin availability and affecting mood circuits. Multiomics links loss of SCFA producers to weaker barrier integrity and altered immune tone.
Some studies note higher Klebsiella aerogenes in premenopausal women with depression and associations between H. pylori and higher symptom scores. Use google scholar to review these subgroup analyses before drawing firm conclusions.
- Balance composition and metabolic data when evaluating evidence.
- Diet and targeted psychobiotics aim to restore function rather than eliminate species.
- Depression often overlaps with anxiety shared mechanisms may explain comorbidity.
Practical tip: consult google scholar for primary studies and mechanistic reports cited in this article before applying interventions.
Bipolar Disorder Schizophrenia and Other Psychiatric Conditions
Cross-diagnostic work highlights repeating patterns: loss of beneficial taxa, gains in pro inflammatory lineages, and altered metabolic output that may affect brain circuits.
Bipolar disorder patterns
Findings: several cohorts report reduced diversity and lower Faecalibacterium with rises in Clostridiaceae, Collinsella, and Actinobacteria related groups. These shifts may reduce SCFA production and weaken barrier support.
Schizophrenia-linked shifts
Studies of schizophrenia note increased Lactobacillus, Collinsella, Succinivibrio, and some Lachnospiraceae. Reductions in Ruminococcus and Roseburia also appear, and metagenome work has flagged Lactobacillus fermentum and Enterococcus faecium in some samples.
Implication: altered composition often coexists with pro inflammatory signals that could modulate immune brain routes.
Autism spectrum features
ASD-related reports frequently find elevated Clostridium paraputrificum, C. bolteae, and C. perfringens. These species-level changes may link to metabolic or toxin pathways implicated in neuro develop mental differences.
- Variability across groups, medications, and comorbidities is large interpretation requires cautious sampling and functional assays.
- Human causal evidence is limited animal models and metagenome studies offer mechanistic clues but need larger cohorts for validation.
Read further: use google scholar to compare studies methods, and replication before applying findings in clinical practice.
Dietary Strategies From Whole Foods to Prebiotics
A Mediterranean-style pattern offers practical scalable ways to support microbial function and mood. A 2017 randomized study linked this diet to reduced depressive symptoms likely via higher fiber and increased short chain fatty acids.

Key dietary elements
Fiber rich plant foods feed SCFA-producing species, bolster barrier integrity, and help immune balance. Tryptophan-rich items (eggs, poultry, legumes) support serotonin pathways and social cognition in some cohorts.
Spices and natural compounds
Curcumin and capsaicin show anti inflammatory effects and modulate community composition in small trials. These natural products act as adjuncts, not replacements, for standard care or probiotics.
| Diet element | Likely effect on microbiota | Implication for mood |
|---|---|---|
| Mediterranean pattern | ↑Fiber, ↑SCFA production | Reduced depressive symptoms (2017 RCT) |
| Prebiotic fiber mix | ↑Bifidobacteria, ↑function | Improved barrier, immune balance |
| Curcumin/capsaicin | Anti-inflammatory shifts | Adjunctive mood benefits |
- Sustained patterns matter: short changes can shift function quickly, durable benefits need long-term intake.
- For study methods and replication use google scholar to verify cohorts and mechanisms.
Practical advice: prioritize whole food variety and fiber diversity to support broad group function consult google scholar for primary reports and this article for summaries. For clinical questions, use google scholar before trying adjunctive probiotics.
Probiotics and Psychobiotics Effects Strains and Adjunctive Use
Clinical teams and researchers have tested live-strain supplements as complements to standard care for mood symptoms. A meta-analysis of seven trials found these supplements effective as add ons for depressive symptoms, but not as standalone treatment.
Human trials show additive improvements in depression and anxiety when probiotics are paired with medications or therapy. A 2023 pilot in partial responders reported larger symptom drops with a multistrain product.
How they may work
Proposed mechanisms include increased serotonin synthesis and production of dopamine and noradrenaline by specific Bacillus strains. Immune modulation and improved barrier support also appear important.
| Strain / mix | Proposed effect | Clinical note |
|---|---|---|
| Lactobacillus + Bifidobacterium | Supports barrier, reduces inflammation | Common in trials; modest biomarker change |
| Bacillus species | May boost dopamine, noradrenaline | Useful adjunct strain-specific |
| Multistrain blends | Broader functional output | Shown to help partial responders (2023) |
Practical points: benefits are heterogeneous and usually adjunctive. Monitor baseline symptoms, align with dietary strategies, and consult clinicians. For primary reports and replication, use google scholar to review trial methods and outcomes.
Fecal Microbiota Transplantation FMT Promise, Limits and Trials
FMT offers a comprehensive route to reset an adult community when targeted approaches fall short. Early pilot programs including work from Valerie Taylor’s team in Calgary aim to test this reset for depression and bipolar disorders.
Clinical experiences and pilot studies
Patient reports from trials, such as a 2023 depression study, describe rapid symptom relief in some people and little change in others. Real world effects are variable, so outcomes must be judged in controlled settings.
Safety donor selection, and unclear mechanisms
Safety depends on rigorous donor screening standardized processing, and clinical monitoring to reduce infectious risks. Regulatory oversight is evolving in the United States.
| Aspect | Current status | Implication for practice |
|---|---|---|
| Clinical trials | Pilot studies, 2023 depression trial, bipolar pilots | Investigational use only in trials |
| Mechanisms | Broad community transfer species attribution unclear | Requires multiomic sampling |
| Preclinical support | Human-to-mice transfers reproduce depressive and anxiety traits | Supports causal role but needs translation |
Given variable response and mechanistic uncertainty, FMT remains an investigational treatment best offered within trials with informed consent. For deeper reading, consult google scholar for trial reports, protocols, and mechanistic follow-up.
Metabolites and Pathways That Bridge Gut and Brain Function
Key small molecules produced by intestinal communities act as messengers that shape barrier integrity, immune tone, and neural signaling.

Short-chain fatty acids and blood-brain barrier integrity
Short chain fatty acids such as butyrate support the blood-brain barrier by strengthening tight junctions and reducing systemic inflammation. Lower SCFA levels link to higher neuroinflammatory markers and altered signaling that can affect mood.
Dietary fiber raises SCFA outputs, which influence immune cells and microglial activation. This pathway shows how metabolites connect intestinal activity to brain function across the axis.
Tryptophan-kynurenine balance and mood regulation
Microbial processing of dietary tryptophan shifts flux between serotonin synthesis and kynurenine metabolites. Some kynurenine derivatives are neuroactive while others are neurotoxic the balance matters for behavior.
Depression related FMT in rodents alters tryptophan metabolism, reinforcing that composition changes can translate into altered circulating levels and downstream effects on the brain.
Measuring metabolites, enzymes, and receptor activity often reveals functional change even when composition looks stable.
Practical research note: prioritize metabolite-focused biomarkers in clinical studies, include species diversity measures for redundancy, and test diet or adjunctive probiotics alongside functional assays. For primary reports and methods use google scholar to locate trials, metabolomics data, and replication studies. Use google scholar again to compare biomarker panels across cohorts, then consult google scholar for mechanistic follow-up cited in this article.
The HPA Axis Inflammation, and Intestinal Permeability
Inflammation and stress hormones interact to erode barrier defenses linking peripheral immune signals to mood circuits.
Cytokines, hormonal cascades, and barrier breach
Elevated IL-6 and TNF-α raise blood-brain barrier permeability and correlate with depressive and anxiety symptoms. Human endotoxin infusion studies induce cytokine surges and transient mood changes, showing immune-to-brain signaling in vivo.
The stress cascade runs CRF → ACTH → cortisol. Chronic hyperactivity of the hpa axis sustains high cortisol levels and amplifies inflammatory signaling. This cycle deepens barrier dysfunction and fuels symptom persistence.
From dysbiosis to systemic inflammation
Dysbiosis promotes intestinal permeability, allowing bacterial products into circulation. That drives cytokine levels up and activates the hpa axis, creating a feedback loop that can maintain symptoms.
Animal work shows certain probiotic regimens lower ACTH and corticosterone and support tight junctions in mice. These findings suggest targeted interventions may reduce hormone levels and improve barrier integrity.
| Pathway | Evidence | Clinical implication |
|---|---|---|
| Cytokine elevation (IL-6, TNF-α) | Human endotoxin and cohort correlations | Monitor cytokine levels where appropriate |
| HPA axis hyperactivity | Consistent in depression models | Combine stress management with adjunctive care |
| Dysbiosis → leaky barrier | Animal transfers, small human studies | Target diet, prebiotics, select probiotics |
- Use google scholar to compare mechanistic reports and biomarkers.
- Given small samples and variable responses, consult google scholar before clinical application.
- Address stress, immune levels, and barrier support together with standard psychiatric care for best translational impact.
How to Read the Research: Studies Samples and Google Scholar Tips
Not all papers carry the same weight study design and sample size shape what conclusions you can trust.
Interpreting study types
Cross-sectional work describes associations in one time point. It can spot patterns but cannot prove cause.
Longitudinal cohorts track changes across time and better support inference about direction. Randomized trials test interventions and give the strongest clinical evidence.
Search strategies and what to prioritize
- Use google scholar filters: date range, citations, and review articles to find meta-analyses.
- Track citations to see how a study influenced later research.
- Prioritize RCTs and meta-analyses for intervention claims use observational work to generate hypotheses.
| Study type | What it shows | Key caution |
|---|---|---|
| Cross-sectional | Associations in a group | No causality |
| Cohort | Temporal trends | Confounders may persist |
| Randomized trial | Intervention effects | Sample size limits generalizability |
Practical tip: look beyond composition to metabolites, immune markers, and endocrine changes when judging whether observed microbiota shifts link to depression or anxiety. Use google scholar to confirm replication and pre registration for stronger evidence in each article.
Personalization and Variability Species Strains and Responders
Not everyone benefits equally from the same strain prior composition and functional redundancy explain much of the variability.
Baseline species composition shapes response. Different communities can substitute for lost roles, so two people with distinct enterotypes may react differently to one supplement.
Strain level specificity matters. Choose psychobiotics for targeted outputs SCFA increase or tryptophan modulation rather than generic labels.
Function can change with little taxonomic shift. Short trials often show altered SCFA output or tryptophan routing before composition moves.
Multiple factors affect who responds: habitual dietary patterns, psychiatric medication use, genetics, and stress levels alter host microbe interactions.
Iterative personalization works best. Monitor symptoms, use functional biomarkers when available, and adjust strains and diet over weeks to months with clinician guidance.
Focus on restoring function rather than chasing specific taxa; replication and careful trials refine who benefits.
| Factor | Typical effect | Clinical implication |
|---|---|---|
| Baseline species array | Alters colonization potential | Tailor strains to missing functions |
| Dietary pattern | Shapes substrate for strains | Combine whole-foods with targeted adjuncts |
| Medications & genetics | Modify response variability | Expect heterogenous responders monitor closely |
| Short-term function shifts | SCFA or tryptophan flux without big composition change | Use metabolites as early readouts |
- Use google scholar to verify strain-specific trials and replicate findings.
- Interpret small studies cautiously larger replication clarifies risk and responder profiles.
- Consult google scholar for protocols that combine dietary foundations with strain selection.
Practical note: personalization is a process. Expect adjustments over months, track outcomes, and use google scholar to guide evidence backed choices in this article’s context.
Clinical and Practical Considerations in the United States
Clinical decisions must balance emerging evidence with regulatory realities and patient safety. Providers should treat gut-directed options as adjunctive approaches, not replacements for standard therapies for depression or other psychiatric disorder.
Regulatory context for supplements and investigational transfers
Probiotics are generally marketed as dietary supplements in the US, so product quality and label accuracy vary. Clinicians should prefer products with third-party testing and documented strains from trials.
FMT remains investigational for psychiatric indications. Outside recurrent C. difficile infection, transfers require formal trial protocols with rigorous donor screening and informed consent.
Working with clinicians: monitoring, safety and shared decisions
Integrate gut directed strategies with pharmacotherapy and psychotherapy under clinician oversight. Use validated scales to track depressive symptoms and set realistic timelines for change.
- Safety monitoring: track adverse events, reconcile medications, and consider stool or blood samples in research settings.
- Product quality: choose tested probiotics and document lot numbers; avoid unverified preparations for vulnerable patients.
- Access and cost: discuss insurance limits, out-of-pocket fees, and trial enrollment as options to access investigational treatment.
| Intervention | US regulatory status | Clinical note |
|---|---|---|
| Probiotics | Supplements variable oversight | Prefer third-party tested strains used in studies |
| FMT for psychiatry | Investigational | Use only in registered trials with donor screening |
| Dietary strategies | Standard care adjunct | Safe, low-cost, broadly recommended |
Practical advice: encourage patients to consider research participation to contribute samples and outcome data. Use google scholar to review trial methods and to inform shared decision-making about risks and likely effect sizes. Refer to google scholar when verifying product claims and when documenting consent for investigational treatment.
Limitations Risks and What We Still Don’t Know
Despite encouraging pilot work large scale confirmation is lacking and uncertainties remain about safety and mechanism.
Small trials and mixed biomarkers: many studies use limited samples, so statistical power is low. Cytokine and BDNF results often fail to track symptom change consistently.
Diagnostic specificity is weak: overlapping pro-inflammatory patterns appear across several disorder groups, so composition changes rarely map to one diagnosis.
Intervention risks: probiotics vary in quality and may interact with psychiatric drugs FMT carries donor variability and unknown long term risk. Careful monitoring is essential.
Early findings are promising but preliminary robust, diverse trials are needed before routine clinical adoption.
- Require larger, longer, and more diverse samples with mechanistic endpoints.
- Track medication interactions and patient centered outcomes in trials.
- Use google scholar to verify replication, pre registration, and effect sizes.
Call to action: fund sustained research and avoid overinterpreting early effect estimates. For clinicians and researchers, consult google scholar to weigh current article claims and guide safe, evidence based use.
Conclusion
Across studies metabolic outputs often explain symptom shifts better than taxonomy alone.
The central finding: the gut links to brain circuits through immune, endocrine, neural, and metabolic routes. This article shows measurable role for community function in mood, including signals tied to SCFAs and tryptophan pathways.
Practical steps: favor whole-food dietary patterns, consider evidence-aligned psychobiotics as adjuncts, and reserve fecal transplant approaches for trials. Personalize care with clinician oversight and monitor outcomes closely to reduce risk.
Limitations remain; larger, longer human studies are needed to clarify who benefits most. Use google scholar to review primary study reports and to track replication. Discuss options with health professionals before trying gut-targeted strategies.