Is magnesiumdeficiency associated with back pain and scleroderma? This question drives a careful, informational review of current research and clinical observations.
magnesium plays a clear role in muscle contraction nerve signaling, bone strength heart rhythm, and energy use. That helps explain why some people link low levels to aching muscles or nerve related complaints.
Evidence ranges from lab-based mechanisms to small clinical studies and reports that touch on autoimmune features. Standard blood tests may not reflect total body status, so clinicians often use multiple clues to assess possible deficiency.
This article stays factual and non diagnostic. It will outline roles of this nutrient, how common inadequate intake is overlapping symptoms possible mechanisms testing options, diet strategies, and safe supplement choices. Expect practical steps you can discuss with your healthcare team.
Key Takeaways
- This article reviews evidence without offering diagnoses.
- magnesium supports muscles, nerves, bones, heart, and metabolism.
- Symptom overlap can make links hard to prove clinically.
- Body levels are tightly regulated testing has limits.
- Discuss diet and supplements with your healthcare provider.
Why magnesium matters now roles prevalence and symptoms
This nutrient supports hundreds of enzymes and helps keep nerves and muscles firing smoothly.
Key body functions: It plays important role in muscle contraction and relaxation, nerve transmission, and ATP production that fuels cells. The mineral also helps form bone and teeth and helps stabilize heart rhythm by reducing excess excitability in muscle and cardiac tissue.
How common are low levels in the United States?
Nearly half of Americans consume less than the estimated average requirement NHANES 2013–2016 . That shortfall raises population level risk for vague, nonspecific symptoms that can be mistaken for other musculoskeletal problems.
Early signs and possible progression
Early symptoms include muscle cramps or twitching nausea fatigue, and reduced appetite. These signs overlap with other causes so clinical review matters.
If low levels persist downstream issues can develop: low calcium or potassium, arrhythmias, and neurologic changes have been reported in more severe cases. Some studies have explored links to neuroinflammatory conditions, but findings remain mixed and require careful interpretation.
- Supports muscle, nerve, and energy function ATP
- Important for bone structure and heart rhythm control
- Influences neurotransmitters and nerve membrane stability
- Many people do not meet intake targets, increasing nonspecific symptom risk
| Function | What it does | Common early signs | Potential severe effects |
|---|---|---|---|
| Muscle & nerve | Supports contraction, relaxation, conduction | Cramps, twitching | Spasms, weakness |
| Energy ATP | Enzyme cofactor for energy metabolism | Fatigue | Reduced exercise tolerance |
| Cardiac & electrolytes | Stabilizes rhythm affects Ca K balance | Palpitations | Arrhythmias, hypocalcemia, hypokalemia |
| Brain & mood | Modulates neurotransmitters, membrane stability | Mood shifts, stiffness | Neurologic changes |
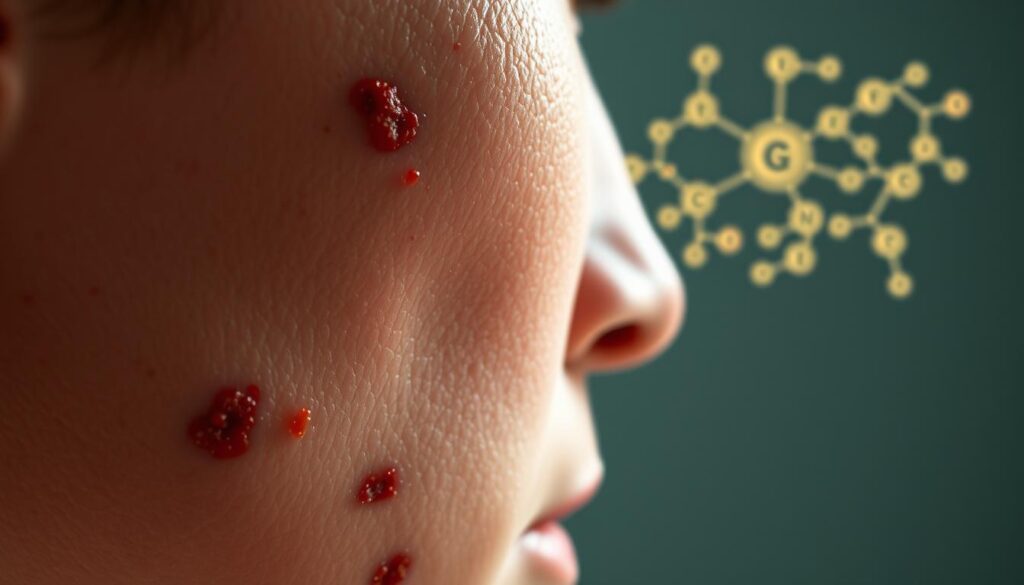
Is magnesium deficiency associated with back pain and scleroderma?
Some clinical and lab studies hint at a link between low mineral stores and neuromuscular symptoms, but evidence varies. This section summarizes what research shows and clarifies symptom overlap so readers can weigh possibilities without drawing firm conclusions.
What current studies and related research suggest
Research is mixed. A few analyses propose that magnesium deficiency may help modulate neuroinflammation and stabilize nerve membranes. Other large studies and cohort work find no clear risk link to central nervous system disorders such as MS.
Available data remain exploratory high-quality, condition specific trials are limited.
Overlap of symptoms: cramps stiffness fatigue and pain
Low levels can cause muscle cramps stiffness tingling numbness fatigue, and mood changes signs that also occur in many chronic musculoskeletal and autoimmune disorders.
Practical point: these shared symptoms can blur diagnosis. Back symptoms are usually multifactorial, so any nutrient role would be one of several modifiable contributors.
If autoimmune disease or systemic signs are suspected medical evaluation is essential. Later sections cover mechanisms testing limits, and safe nutrition steps to discuss with your clinician.

How low magnesium may contribute to back pain
When tissue stores run low, nerve membranes may fire more easily and muscles can tighten around the spine. That shift in excitability can cause spasms or sustained tension that mimic or worsen spinal complaints.
Muscle tension spasms and neuromuscular conduction
Low levels increase muscle excitability which raises the chance of cramps twitching, and guarding. These signs may limit range of motion and create painful trigger points in paraspinal muscles.
Central nervous system sensitization and chronic pain
Persistent overstimulation of pain pathways can amplify discomfort over weeks to months. Reduced mineral support has been discussed as one factor that may promote central sensitization seen in chronic spinal syndromes.
When to consider other causes
Blood tests can underestimate tissue shortfalls because most of this element sits inside cells and bone. If cramps or refractory stiffness continue despite standard care, clinical evaluation is reasonable.
- Multiple drivers often underlie spinal symptoms disc joint nerve compression inflammation, or myofascial issues.
- Red flags: progressive weakness fever unexplained weight loss, severe neurologic loss, recent trauma, or cancer history seek urgent care.
- Stepwise plan: address biomechanics PT movement sleep and stress and discuss nutritional assessment with your clinician when muscle signs persist.
Magnesium and autoimmune connective tissue disorders: implications for scleroderma
Autoimmune connective tissue conditions have spurred study of nutrient pathways that affect inflammation, immune signaling, and tissue repair. Interest centers on whether targeted support could ease symptoms or slow progression.
Inflammation, the central nervous system, and potential anti‑inflammatory effects
Some recent research suggests that certain minerals may reduce neuroinflammation and modulate nerve signaling in the central nervous system. A 2022 article reported possible benefits for neurodegenerative pathways, while other long-term work found no clear link to MS risk.
Practical takeaway: reduced cellular stores might influence fatigue and pain processing, but evidence is mixed and often indirect.
Cautions: conflicting evidence and clinician guidance
Comparative studies and reviews sometimes show no meaningful difference in levels between affected groups and controls. That conflict means overgeneralizing benefit is risky.
No conclusive evidence ties levels directly to scleroderma outcomes.
- Magnesium supports vitamin D activation combined optimization helped in some MS studies.
- People with autoimmune disorders should consult rheumatology before starting supplements.
- Monitor overall nutrition and systemic inflammation as part of care.
| Area | Evidence | Clinical note |
|---|---|---|
| Immune regulation | Biologic rationale few disease-specific trials | Interest exists but direct scleroderma data are limited |
| Central nervous system | Some studies show reduced neuroinflammation in models | Extrapolate cautiously to clinical symptoms |
| Vitamin interaction | Supports vitamin D metabolism | Combined optimization may help selected patients |
Checking your status: limits of blood tests and better ways to assess magnesium levels
Serum testing offers a narrow view. Less than 1% of total body stores circulate in blood, so routine labs can appear normal even when tissue reserves are low.
Clinical signs matter. People who have persistent cramps, heart rhythm changes, or stubborn musculoskeletal symptoms may need more than a basic serum check.
Why serum can miss tissue shortfalls
The body maintains stable blood values by pulling from bone and muscle. That homeostasis masks early or chronic depletion at the cellular level.
Alternative assessments clinicians may use
- Red blood cell testing: suggests intracellular status.
- 24-hour urinary excretion: reflects recent intake and losses.
- Oral or IV loading tests: evaluate retention versus loss after a controlled dose.
- Hair, muscle, or bone analysis and EXA: measure longer-term stores in tissues.
- Ionized-to-total ratio: may uncover physiologic imbalance missed by total serum values.
Test choice is individualized. Discuss pros, cons, costs, and how results will change management with your clinician before proceeding.
Increase magnesium levels safely foods intake targets and absorption tips
A food-first approach can help most adults reach recommended intake targets without supplements.
Practical grocery choices matter. Build a shopping list that centers on seeds, nuts, legumes, whole grains, leafy greens, dairy, and soy products to increase magnesium levels through everyday meals.
Easy additions: pumpkin seeds, chia seeds, almonds, spinach, black beans, edamame, brown rice, and low fat plain yogurt. These items provide measurable milligrams per serving and also add fiber and protein to the diet.

Recommended daily allowance and who may need closer attention
Adults: aim for about 310–420 mg/day depending on age and sex. Track intake for several days to spot gaps before considering supplements.
People at higher risk for low levels include older adults, those with gastrointestinal disorders, type 2 diabetes, or users of PPIs, diuretics, bisphosphonates, or certain antibiotics. Discuss testing and drug interactions with your clinician.
Improving absorption and plate-building ideas
Correct low vitamin D when present, since vitamin status helps absorption. Avoid unnecessary high-dose zinc, which can interfere with mineral uptake.
- Add seeds to oatmeal or yogurt in the morning.
- Use brown rice or quinoa as a side instead of white rice.
- Include a leafy salad or sautéed spinach at lunch and dinner.
- Rotate legumes black beans, edamame, and lentils for variety.
| Tip | Example serving | Approx. mg per serving | Why it helps |
|---|---|---|---|
| Seeds | 1 oz pumpkin seeds | 156 mg | High concentration easy snack or topping |
| Nuts & dairy | 1 oz almonds / 8 oz yogurt | 80 mg / 42 mg | Portable sources with protein and calcium |
| Legumes & grains | ½ cup black beans / ½ cup brown rice | 60 mg / 42 mg | Staples that boost intake across meals |
| Greens & soy | ½ cup boiled spinach / 1 cup soymilk | 78 mg / 61 mg | Leafy greens and plant milks improve daily totals |
Food-first strategies deliver multiple nutrients that support bone, muscle, and heart health. If tracking shows persistent shortfalls or you take medications that increase losses, talk to your healthcare provider about next steps.
Choosing magnesium supplements forms benefits and side effects
Choosing the right supplement form affects how well your body absorbs this essential mineral. Match the product to your goal sleep, muscle ease, heart rhythm support, or brain focus to improve results and reduce side effects.
Bioavailable options
Citrate and glycinate are highly absorbable. Citrate often eases constipation but can loosen stools. Glycinate is gentle and commonly chosen for relaxation and sleep.
Chloride, malate, taurate, and L‑threonate target specific needs: electrolyte balance, muscle energy, heart rhythm support, and brain penetration, respectively.
What to know about oxide and GI effects
Oxide is poorly absorbed and mainly acts as a laxative. Avoid relying on it for repletion unless a clinician recommends it for that effect.
Oral vs transdermal: evidence and expert view
Small studies on topical oils or Epsom baths show mixed results. Experts prefer food-first and oral routes for predictable increases in levels.
Safety and when to seek advice
Start low and titrate to limit GI effects. Space supplements from certain drugs and avoid high doses if you have kidney disease, are elderly, or care for infants. Recheck blood or intracellular testing when clinically indicated and discuss plans with your provider.
| Form | Main benefit | Common side effect |
|---|---|---|
| Citrate | Good absorption eases constipation | Loose stools |
| Glycinate | Gentle supports relaxation and sleep | Rare GI upset |
| L‑threonate | Crosses blood brain barrier cognitive focus | Limited long term data |
| Oxide | Laxative effect low repletion value | Diarrhea poor absorption |
Conclusion
A practical plan focused on diet, careful testing, and clinician guidance offers the best route to improve symptoms tied to poor mineral status.
Address intake first. Prioritize foods such as pumpkin seeds, nuts, legumes, leafy greens, whole grains, and dairy to boost daily totals and support muscle and nerve function.
Recognize that blood tests may miss tissue shortfalls. If cramps, stiffness, or fatigue persist, ask a clinician about more specific tests and whether targeted supplements are appropriate.
Use supplements thoughtfully, consider comorbid conditions diabetes, kidney issues , and reassess levels after changes. Adequate intake also supports heart rhythm, bone health, and overall system function.
This article is informational, not diagnostic. Work with a healthcare professional to tailor strategies that reduce risk and support function for your unique conditions and symptoms.





