Can a small piece of fruit really help keep blood sugar steady, or is fruit always a risk?
This guide shows how whole fruit can fit into a diabetes-friendly eating plan without spiking levels.
Scientific guidance from trusted U.S. sources supports choosing fresh or frozen options, watching portions, and pairing fruit with protein or healthy fats.
The picks ahead focus on low-to-moderate glycemic impact, meaningful fiber, and nutrient density vitamins, potassium, and antioxidants to support overall health and steady blood glucose.
Whole fruit often beats juice because fiber slows sugar absorption and helps you feel full.
Below the image, you’ll find clear serving visuals, calorie and carb data, and practical tips to make fruit part of a smart diabetes care plan.
Key Takeaways
- Whole fruit can be included in a diabetes meal plan when portions are controlled.
- Choose fruits with fiber, vitamins, and antioxidants to help steady blood sugar.
- Favor fresh or frozen fruit without added sugar limit juice and dried fruit.
- Pair fruit with protein or healthy fats and space servings through the day.
- Monitor personal response and consult a registered dietitian or diabetes educator.
Why Whole Fresh Fruits Belong in a Diabetes Diet Today
Whole, intact fruit can be a smart part of a diabetes meal plan when chosen and portioned correctly.
Whole fruits slow sugar absorption. Fiber, water, and the fruit’s intact cell structure blunt fast rises in blood glucose and help you feel full. The Cleveland Clinic notes that fiber slows digestion and supports more gradual glucose increases.
The American Diabetes Association highlights berries as nutrient-dense choices. For example, one cup of blueberries has about 84 calories and 21 grams of carbohydrates, per USDA data. These berries add antioxidants and vitamins without huge sugar loads.

- Prioritize fresh or unsweetened frozen fruit over juice to keep fiber intact.
- Aim for two fruit servings a day, spaced across meals and snacks.
- Eat a variety of colors to maximize vitamins, phytonutrients, and heart health benefits.
Fiber slows digestion, supporting more gradual glucose rises and reducing the likelihood of sharp spikes in blood.
Monitor your own blood response and work with USDA FoodData Central or an RD to tailor choices to medications and activity.
Glycemic Index, Fiber, and Portion Size: What Regulates Blood Sugar
How quickly a fruit raises glucose depends on its glycemic behavior and portion size.
Low glycemic index fruits and steady blood sugar levels
The glycemic index measures how fast foods raise blood sugar after you eat them. Lower numbers mean smaller, slower spikes in glucose.
Low glycemic choices many berries and citrus tend to keep levels steadier and can reduce demand on insulin during the day.
Fiber’s role in slowing carbohydrates and protecting heart health
Fiber slows carbohydrate breakdown and absorption. That flattens glucose curves and helps you feel full.
Soluble fiber also supports heart health by improving cholesterol. Pairing a smart serving with protein or healthy fat slows sugar absorption further.
- Practical serving: a tennis ball–size fruit or about 3/4–1 cup cut fruit is a useful serving size to regulate blood sugar.
- Track your response: check blood before and 1–2 hours after eating to see how your body reacts.
- Remember: both total carbohydrates and glycemic qualities matter in a balanced diet.
Choose whole fruit and right-size servings to help regulate blood and support long-term diabetes control.
Criteria We Used to Choose Diabetes‑Friendly Fruits
We ranked options by nutrient density, carbohydrate content, and how easy each is to portion in daily life.
Nutrition profile: vitamins, antioxidants, and calories per serving
Priority went to fruits that deliver vitamins and antioxidants while keeping calories reasonable. Fruits with vitamin C, vitamin A, potassium, and notable antioxidant content earned higher marks.
We favored whole, skin‑on options to boost fiber and nutrient content without added sugar. This supports overall health and steadier blood sugar levels.
Carbohydrates, grams per cup, and practical serving size
Carbohydrate totals in grams per cup or per small fruit guided portion recommendations. We used USDA values to compare grams and calories so servings fit common carbohydrate budgets.
Practical serving size aims near a tennis ball or about 3/4–1 cup diced. That size is easy to track and pairs well with protein or a healthy fat to blunt glycemic rises.
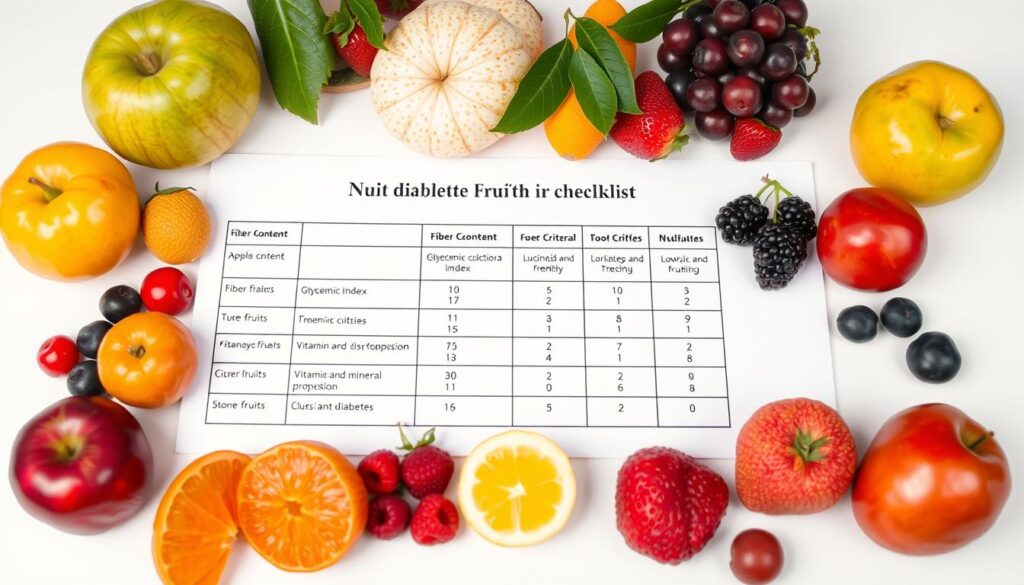
Use measured servings and whole fruit to get nutrients without large sugar spikes.
| Fruit | Typical serving | Calories | Carbs g |
|---|---|---|---|
| Blueberries | 1 cup | 84 | 21 |
| Tart cherries | 1 cup with pits | 52 | 12.6 |
| Peach | 1 medium | 59 | 14 |
| Apricot | 1 small | 17 | 4 |
| Apple | 1 medium skin on | 95 | 25 |
Top 7 Fruits for Diabetics
Choosing the right fruits makes it easier to enjoy natural sweetness without large blood sugar swings.

Berries Blueberries and strawberries pack antioxidants and fiber that help blunt post‑meal glucose rises. One cup of blueberries has about 84 calories and 21 grams of carbs, making measured servings easy to fit into a diabetes plan.
Tart cherries offer anti‑inflammatory antioxidants. A cup with pitscontains near 52 calories and 12.6 grams of carbs, so a small bowl or yogurt topping adds flavor with modest sugar.
Peaches provide potassium and vitamin C with moderate carbs about 59 calories, 14 grams . They work well sliced into salads or unsweetened drinks.
Apricots are fiber‑rich bites four give roughly 3 grams of fiber and meaningful vitamin A, useful in oatmeal or salads without excess sugar.
- Apples skin oncontribute 4 g fiber per medium fruit and antioxidants that support steadier blood measures.
- Citrus oranges and grapefruit bring vitamin C, folate, and a lower glycemic impact than juice eat whole segments, not the juice.
- Kiwis are low‑calorie, about 48 calories each, with vitamin C and fiber for quick, portion‑perfect additions.
Favor whole, measured servings to harness fiber benefits and keep the glycemic response gentler.
Serving Sizes That Help Manage Blood Sugar Levels
Simple portion rules let fruit fit into a diabetes meal plan while keeping sugar levels steady.
Visual size matters. A small to medium piece roughly the size of a tennis ball or about 3/4–1 cup of cut fruit equals one serving for most choices.
What a cup, a small fruit, or a tennis ball portion looks like
One serving often delivers about 15–25 grams of carbohydrates. For example, one cup blueberries 21 grams one medium apple 25 grams one medium orange 16 grams.
Use a measuring cup at first to train your eye. Dried fruit is concentrated just a few tablespoons can equal a full fresh serving.
Spacing fruit across meals and snacks in your daily plan
Space two fruit servings across the day for instance, breakfast and midafternoon rather than eating both at once. This helps smooth blood sugar levels and reduces insulin demand after a meal.
- Pair a serving with protein or healthy fat Greek yogurt, nuts to blunt quick rises.
- Split larger items half an apple now, half later to keep carbohydrates balanced between meals.
- Check your blood after new combinations to fine‑tune portion choices for your body.
Measure early, estimate confidently later, and space servings to support steady blood control.
| Portion | Visual | Approx. carbs g |
|---|---|---|
| 1 medium apple | Tennis‑ball size | 25 |
| 1 cup blueberries | 1 cup cut | 21 |
| 1 medium orange | 1 cup segments | 16 |
Smart Ways to Add Fruit to a Diabetes Meal Plan
Small swaps in meals make it simple to enjoy fruit while keeping glucose stable.
Pair fruit with protein or healthy fats to slow sugar absorption and reduce insulin demand. Try plain Greek yogurt with 1/2–1 cup berries for a breakfast parfait that adds fiber and antioxidants while offering steady protein.
Build balanced meals. Toss orange segments or sliced pear into a salad with leafy greens, nuts, and a light vinaigrette. The mix of fiber and fat lowers glycemic impact and boosts nutrients and flavor.
Breakfast, salads, and smoothies without added sugar
Make smoothies with whole fruit, plain yogurt or protein powder, and a spoon of nut butter or avocado. Skip juice and added sweeteners to preserve fiber and avoid fast sugar spikes.
Use fruit as a topper rather than a base: sprinkle diced apple or kiwi over oatmeal or chia pudding to add natural sweetness plus fiber.
Fresh and frozen options for year‑round access
Choose fresh or unsweetened frozen fruit to keep fiber intact. Frozen berries, peaches, and kiwi are convenient and retain most nutrients.
Pre-portion 1-cup servings into containers for easy snacks. Rotate colors to get varied antioxidants and nutrients and to make your plan sustainable.
Pairing fruit with protein and healthy fat helps control blood sugar and makes sweet choices work within a diabetes-friendly diet.
| Use | Example | Why it helps |
|---|---|---|
| Parfait | Plain Greek yogurt + 1/2–1 cup berries | Protein + fiber blunts sugar rise |
| Salad topper | Orange segments + nuts + greens | Fiber and healthy fat lower glycemic effect |
| Smoothie | Whole fruit + protein + healthy fat | No added sugar slower digestion |
Fruits and Formats to Limit for Better Blood Sugar Control
Some fruit formats pack sugar so tightly that a few bites can raise blood sugar quickly.
Dried fruit and fruit juice concentrate natural sugar and lack the fiber of whole fruit. The ADA warns that small portions like a couple tablespoons of raisins can equal a significant carb load. If you drink juice, cap it near a 1/2 cup and always pair it with protein to slow absorption.
High‑glycemic choices to limit include watermelon, mango, pineapple, and large handfuls of grapes. These have a higher glycemic index and can spike sugar levels when eaten in big portions. Keep servings small and balance them with healthy fat or protein.
Canned fruit and applesauce can be okay if labeled no added sugar or packed in juice rather than syrup. Read ingredient lists added sweeteners raise calories and sugar content and increase risk to blood sugar control and heart disease over time.
- Measure dried cherries and other dried fruit 1–2 tablespoons, not a handful.
- Favor whole citrus like grapefruit and oranges over juice to keep fiber and steady glycemic response.
- Pre-portion higher‑GI fruit and pair with nuts, cheese, or yogurt to blunt sugar rises.
Choose unsweetened, whole, and well‑portioned fruit formats to help maintain steadier blood sugar.
Safety Tips for People in the United States Managing Diabetes
Practical safety steps help people in the United States keep fruit choices from causing unexpected glucose spikes.
Read labels carefully. Scan ingredient lists for added sugars, syrups, or flavored cups. Pick canned fruit packed in juice and natural applesauce labeled no added sugar.
Compare nutrition facts to check total and added sugar per serving. Watch portion sizes dried fruit is concentrated and a small spoonful can match a whole fresh fruit.
Work with a specialist
Partner with a U.S.-based registered dietitian nutritionist RDNor a diabetes care and education specialist CDCES. Bring glucose data to appointments so your clinician can help you regulate blood sugar and coordinate fruit timing with medications and activity.
Bring your glucose data to refine choices that regulate blood and support steady levels.
- Keep shelf-stable, unsweetened options for convenience without added sugar.
- Build a simple weekly plan that slots fruit into meals and snacks to control blood sugar.
- Revisit your strategy as medications, activity, and goals change.
| Label tip | Action | Why it helps |
|---|---|---|
| Check ingredients | Choose no added sugar or juice-packed cans | Reduces hidden sweeteners that raise sugar levels |
| Compare facts | Note serving size and added sugar grams | Matches portions to your meal plan and glucose targets |
| Measure dried fruit | Use small portions 1–2 tbsp | Prevents concentrated carbs from spiking blood |
| Use clinician data | Share pre/post glucose readings | Personalizes fruit timing and portions to manage blood |
Conclusion
Smart choices make fruit a practical part of daily diabetes care. ,
Choose whole, fresh or unsweetened frozen fruit in measured servings to get fiber, vitamins, and antioxidants without extra calories or concentrated carbohydrates. Pair servings with protein or healthy fat to blunt sugar levels and favor lower‑glycemic picks from the list.
Use simple visuals a tennis ball or a measured cupand limit juice or large amounts of dried fruit. Monitor your blood before and after new combinations and work with an RDN or CDCES to tailor a meal plan that fits your body, meds, and goals.
When you focus on portions, pairing, and format, fruit can support steady blood readings and long‑term heart and metabolic health for people living with diabetes.





